Key Points
- Parkinson’s disease, DLB, and MSA involve misfolded α-synuclein aggregation, but their similar symptoms hinder accurate diagnosis—especially early on. Seeding assays that detect α-synuclein aggregation in CSF offer improved specificity.
- While total α-synuclein levels in plasma have limited diagnostic use, ongoing research is investigating whether disease-specific modifications, such as phosphorylation and truncation, could make plasma α-synuclein a viable CNS biomarker.
- A novel MS-based method allows quantification of non-modified α-synuclein peptides in plasma, offering an indirect but powerful strategy to detect disease-specific molecular signatures across α-synucleinopathies.
Parkinson’s disease and related disorders such as dementia with Lewy bodies (DLB) and multiple system atrophy (MSA) are collectively known as α-synucleinopathies, characterized by the accumulation of misfolded α-synuclein protein in the brain. Differentiating between these conditions is challenging due to overlapping symptoms, especially in early stages. Emerging diagnostic tools like seed amplification assays and neurofilament light chain measurements show promise in detecting disease-specific patterns of α-synuclein aggregation in cerebrospinal fluid. However, plasma α-synuclein has shown limited diagnostic value due to its high expression outside the brain. Recent findings suggest that disease-specific truncations and post-translational modifications of α-synuclein, especially phosphorylation at key residues, may provide more accurate biomarkers. LCGC International spoke to Pablo Mohaupt, who, along with Marie-Laure Pons and their colleagues at the Clinical Proteomics Platform of Montpellier (Montpellier, France) and Shimadzu Corporation (Duisburg, Germany) developed a mass spectrometry (MS)-based method to measure α-synuclein peptides in plasma, aiming to identify disease-specific biochemical signatures that could support earlier and more precise diagnosis of α-synucleinopathies. The team’s efforts have inspired a recent paper published in Brain Communications (1).
How do α-synuclein aggregation patterns differ between Parkinson’s disease, dementia with Lewy bodies (DLB), and multiple system atrophy (MSA), and why is this distinction clinically important?
Although all three disorders are α-synucleinopathies, they differ in how α-synuclein aggregates, both in terms of cellular localization and filament structure. In PD and DLB, α-synuclein aggregates into Lewy bodies and Lewy neurites, primarily within neurons. The aggregated α-synuclein adopts the Lewy fold, a conformation that includes at least amino acid residues 31 to 100. This fold is characteristic of PD and DLB. In contrast, in MSA, α-synuclein aggregates primarily in oligodendroglial cells, and the resulting fibrils adopt distinct structural folds. MSA filaments are composed of two types of protofilaments, either PF-IA and PF-IB or PF-IIA and PF-IIB. These protofilaments have a structured core but differ in how they fold and interact. Their conformation is unique to MSA. These structural differences are clinically important because they suggest that the underlying mechanisms of aggregation, including proteolytic processing, conformational seeding, and cellular context, may differ between these diseases. Understanding these distinctions is essential for developing diagnostic tools and targeted therapies.
What is the principle behind seed amplification assays, and how have they contributed to improving diagnostic differentiation among α-synucleinopathies?
A key pathogenic mechanism in α-synucleinopathies is known as seeding, where misfolded α-synuclein fibrils recruit soluble monomers and promote their conversion into new aggregates. Seed amplification assays (SAAs) directly model this self-propagation process in vitro. They take advantage of the fact that disease-associated α-synuclein can act as a template to induce the misfolding and aggregation of recombinant α-synuclein. By adding patient-derived seeds to a solution of normal α-synuclein and applying cycles of agitation, the assay mimics the templated aggregation that occurs in disease. Aggregation is tracked in real time using a dye, which fluoresces when bound to the fibrils. The resulting signal reflects the presence and seeding capacity of misfolded α-synuclein. SAAs have significantly improved diagnostic capabilities. They can detect pathological α-synuclein in cerebrospinal fluid, even in early disease stages. Moreover, different α-synucleinopathies show distinct seeding kinetics and aggregate properties, which makes it possible to differentiate. SAAs help refine diagnosis and patient stratification based on underlying biology rather than clinical features alone.
What challenges are associated with relying solely on clinical diagnosis for differentiating Parkinson’s disease, DLB, and MSA in early stages?
The primary diagnostic approach for these conditions is clinical, but early symptoms often overlap. DLB is diagnosed when cognitive symptoms appear before or at the same time as motor symptoms, while Parkinson’s disease typically begins with motor signs and may lead to cognitive decline later. MSA is identified based on clinical features and MRI findings, but in early stages it can resemble Parkinson’s disease. These diagnoses depend on subtle differences in symptom timing and progression, which are often difficult to determine accurately. This can lead to misclassification. This makes clinical diagnosis alone an unreliable basis for early detection or patient selection in therapeutic trials.
Your study explored non-modified α-synuclein peptides in plasma. Why did you choose this approach over targeting post-translational modifications directly?
We focused on non-modified α-synuclein peptides because they offer a practical starting point for developing a robust and reproducible plasma assay. Targeting post-translational modifications, can provide valuable disease-specific information, but these modified forms are often present at low levels and can be technically challenging to detect reliably. By measuring non-modified peptides of α-synuclein we aimed to capture indirect signatures of disease-related processes. For example, certain truncations or modifications may lead to decreased levels of the corresponding non-modified peptide. A limitation of this strategy is that if modified forms are present in very low abundance, the resulting changes in non-modified peptides may be too subtle or diluted to detect. This is particularly relevant in our study, where we observed relatively high coefficients of variation for several peptides, which may have further masked group differences. Therefore, our results do not rule out the presence of disease-specific post-translational modifications. It also served as a foundation for future work. Now that we have established this method, we can build on it to include targeted detection of modified peptides, which may provide more specific insights into disease mechanisms.
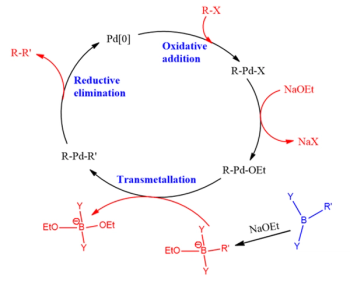
How did the use of liquid chromatography-mass spectrometry (LC-MS) enable you to assess peptide distribution across different α-synucleinopathies in plasma samples?
LC–MS/MS allowed us to selectively and quantitatively measure individual peptides from different regions of the α-synuclein protein in plasma. Using a targeted multiple reaction monitoring approach, we could assess peptides from the N-terminal and NAC domains with high specificity, even in a complex matrix. Unlike immunoassays, which typically provide a single total protein readout, LC–MS/MS enabled us to compare the relative abundance of specific peptides along the α-synuclein sequence. This made it possible to investigate whether certain regions were differentially processed or represented in different α-synucleinopathies. Additionally, the use of LC–MS/MS avoids potential issues related to antibody binding, such as interference from post-translational modifications that can mask epitopes.
What were the key findings regarding the α-synuclein peptide 61–80, and what do they suggest about potential regulatory differences in MSA?
First, I would like to emphasize the exploratory nature of this study. These findings must be interpreted with caution. The MSA group was small and not balanced in size relative to the other groups, which limits statistical power. We also observed relatively high coefficients of variation for several peptides, which may have masked subtle differences or introduced variability. In addition, we did not include a separate validation cohort, which would be necessary to confirm these observations. Despite these limitations, the α-synuclein peptide spanning residues 61 to 80, located within the NAC domain, showed a different abundance pattern in MSA compared to Parkinson’s disease, DLB, and controls. This peptide contributed more strongly to classification models involving MSA, suggesting it may be differentially regulated in this condition. Because the NAC domain is critical for α-synuclein aggregation, changes in this peptide could reflect disease-specific differences in proteolytic processing, aggregation dynamics, or post-translational modifications. These findings have to be investigated further in larger, well-characterized cohorts with improved assays.
What are the implications of your findings that the N-terminus and NAC domain peptide levels remain consistent across α-synucleinopathies?
Our results show that the non-modified peptides display similar levels in plasma across PD, DLB, and MSA. However, this does not rule out disease-specific differences. Because we analyzed plasma, which contains high peripheral α-synuclein, central nervous system–specific signals may be diluted. Additionally, while non-modified peptides can reflect underlying changes such as truncation or post-translational modification, those effects may be subtle and not detectable with our current sensitivity. Therefore, the lack of differences can also reflect both biological complexity and methodological limitations, rather than the absence of disease-specific processes.
Given the extensive peripheral expression of α-synuclein, particularly in erythrocytes, what strategies might overcome the dilution effect observed in plasma-based biomarker studies?
Cerebrospinal fluid (CSF) remains the most reliable source for detecting central nervous system pathology, as it contains less peripheral α-synuclein and has shown strong diagnostic performance in seed amplification assays. In plasma, one strategy is to isolate neuronally derived extracellular vesicles, which are more likely to contain CNS-origin α-synuclein and can reduce background from erythrocytes. Another is to focus on post-translational modifications or disease-specific conformations. Once these features are confirmed in CSF or extracellular vesicles, they can guide the development of more targeted and specific assays in blood.
How might future MS workflows benefit from targeting phosphorylated or truncated α-synuclein forms, and what MS techniques would be best suited for this?
Because these species are typically present at low abundance, initial work should be done in cerebrospinal fluid, where central nervous system signals are more concentrated and peripheral interference is reduced. If robust signatures are identified in CSF or extracellular vesicles, assays can be adapted for blood using enrichment techniques. A clear example of this approach is the use of mass spectrometry to quantify phosphorylated tau at threonine 217 (p‑tau217), a low-abundance but disease-relevant form of tau. In that case, a parallel reaction monitoring (PRM) method on a high-resolution mass spectrometer enabled reliable detection and quantification in both CSF and plasma. For α-synuclein, both PRM and multiple reaction monitoring (MRM) are viable options. PRM is useful during the discovery phase or when precise localization of a modification is needed. MRM, typically performed on triple quadrupole platforms, is better suited for high-throughput quantification once target peptides and transitions are well defined.
To what extent do you believe mass spectrometry can be standardized and scaled for routine clinical use in the differential diagnosis of α-synucleinopathies?
I believe mass spectrometry plays a critical role in the discovery phase of biomarker development, particularly for identifying disease-specific forms such as phosphorylated or truncated α-synuclein. It offers high specificity, the ability to distinguish between modified and non-modified peptides, and detailed structural resolution that is essential for understanding disease mechanisms. However, for large-scale clinical implementation, ultra-sensitive immunoassays are likely to be more practical. Technologies such as Single Molecule Array (Simoa) and NUcleic acid Linked Immuno-Sandwich Assay (NULISA) are already capable of detecting low-abundance proteins and modified proteins with high throughput and may eventually be adapted to target the specific forms of α-synuclein identified through mass spectrometry. In this sense, I see mass spectrometry and immunoassays as complementary. MS is essential for discovery and characterization, while immunoassays are better suited for routine screening and diagnosis once specific targets are validated.
How could isotope-labeled standards or peptide enrichment strategies improve the sensitivity and specificity of MS-based detection of disease-relevant α-synuclein peptides?
Isotope-labeled standards are essential for accurate and reproducible quantification of peptides and proteins with mass spectrometry. By co-eluting with the endogenous peptide and serving as an internal reference, they allow for precise correction of variability in, for example, ionization efficiency and sample handling. This improves both the sensitivity and the specificity of peptide detection, particularly in low-abundance targets. Peptide enrichment strategies can further enhance detection by reducing the complexity of the sample. This includes immunoprecipitation using antibodies, as well as fractionation methods that isolate aggregates, peptides, or extracellular vesicles.
References
- Pons, M. L.; Mohaupt, P.; Vialaret, J. et al. Plasma α-synuclein Domain Profiles Across α-synucleinopathies. Brain Commun. 2025, 7 (3), fcaf189. DOI: 10.1093/braincomms/fcaf189