- October 2023
- Volume 36
- Issue 09
- Pages: 361–368
Good Laboratory Practice: An Overview for the Analytical Chemist
An overview of GLP regulations and related public standards.
Good Laboratory Practice (GLP) is a regulatory requirement to help ensure the quality, reliability, and integrity of pharmacological and toxicological studies during drug development. This article overviews GLP regulations and related public standards, focusing on practices relevant to analytical and bioanalytical chemists.
Nonclinical and clinical studies are the two pillars of new drug development (1,2). Many of these studies are regulated by health authorities, as described in our previous overview article on pharmaceutical regulations (3). Here, we discuss Good Laboratory Practice (GLP) regulation described in Title 21 Code Federal Regulations (CFR) Part 58 (4), enacted in 1978 to ensure data accuracy and integrity of nonclinical laboratory studies (5–8). Two types of mandatory nonclinical studies conducted in the preclinical stage on new molecular entities (NMEs) are pharmacology/drug disposition and toxicology (safety) evaluations. Pharmacology/drug disposition studies investigate the pharmacological effects and the mechanisms of action of the drug in animals, providing information on the absorption, distribution, metabolism, and excretion (ADME) of the investigational product (9,10). Toxicology studies monitor the toxicological effects of the drug in vitro (cell cultures) and in vivo (animals) (11).
While GLP regulations are requirements for conducting pivotal nonclinical safety studies before first-in-human clinical trials, the principles and practices of GLP are often adopted and combined with Good Clinical Practice (GCP) (12,13) for clinical bioanalytical testing (such as those tests for blood, plasma, urine, or tissues collected from test subjects during clinical trials). These public standards are known as Good Clinical Laboratory Practice (GCLP) (14,15).
This paper highlights the principles and practices of GLP relevant to both analytical and bioanalytical chemists supporting nonclinical studies.
Table 1 lists the terms and acronyms used in the paper.
GLP in Drug Development and Registration of Other Products
GLP is a quality system covering the required organizational processes and the conditions under which pivotal nonclinical studies are planned, performed, monitored, recorded, reported, and retained (4,5). GLP studies are required to register new chemicals, food, colour additives, human and animal drugs, medical devices, biological products, biocides, or agrochemicals (4,5). This paper focuses on drugs for human use. However, agencies such as the United States Environmental Protection Agency (EPA) also issue GLP regulations for products under their purview (16), as promulgated in 40 CFR 160 (FIFRA) and 40 CFR 792 (TSCA).
Regional authorities such as the FDA, EMA, and OECD establish GLP regulations for human-use drugs. In the USA, the FDA has published the GLP in the Code of Federal Regulations (CFR) – Title 21 CFR Part 58 (4). Currently, OECD has 38 member countries that have adopted the OECD GLP principles and guidance documents (8). There are EU directives relating to adopting GLP principles, some of which reference OECD-published guidelines (17,18). While there are many similarities between regional GLP regulations, not all aspects are the same, especially for terminologies (19). As described in a previous paper (3), it is incumbent on the sponsor to fully understand the regulations within the jurisdiction they wish to conduct studies.
We will briefly discuss pharmacokinetic (PK) and toxicokinetic (TK) studies, which are nonclinical studies that aim to demonstrate that the drug candidate is safe for initial human testing and exhibits the desired pharmacological activities. Before the drug can be tested in humans, GLP preclinical PK studies should be performed in rodent and non-rodent species. PK studies determine the concentration of the drug candidate within various parts (organs) of the animal at defined time points after drug administration. PK studies aim to obtain bioavailability data (how the drug is absorbed into the systemic circulation) and to allow extrapolation to human equivalent doses (9–11). TK studies also determine the concentration of the drug within different parts of the animal at defined time points after administration of the drug. They are designed to aid the interpretation of toxicity findings. TK studies use exaggerated concentrations of the drug candidate to study how toxic the drug may be (maximum tolerable dose). Preclinical toxicology studies often comprise acute (single dose), subacute (repeat dose), genotoxicity, and safety pharmacology studies. A 28-day repeat dose toxicology study in rodents and non-rodents is typically needed before investigational new drug (IND) application for human clinical trials (11,20).
In addition to preclinical PK and TK studies for safety evaluation that should be conducted under GLP, other studies may include general toxicity studies (acute, sub-chronic, and chronic), local tolerance studies, genotoxicity studies, carcinogenicity studies, developmental and reproductive toxicity studies, immunotoxicity studies, analytical studies of biological sample collected from animals, and analytical studies of the dose formulations (21).
Table 2 lists 10 principles of GLP according to OECD, with brief descriptions of each (4,8). The reader is referred to the official guidance documents and the company’s internal standard operating procedures (SOPs), if available.
GLP vs. cGMP
While GLP and current Good Manufacturing Practice (cGMP) regulations have similar goals to ensure data accuracy and integrity and are enforced by the FDA in the USA, there are significant differences (3–5). GLP applies to the preclinical or nonclinical safety testing phase of drug development and focuses on short-term projects and standalone studies often conducted in contract research organizations (CROs) (22). The principles of GLP are adopted and followed in bioanalytical testing in clinical studies. cGMP regulations apply to the late-stage drug manufacturing process of drug substances and products, including clinical trial materials and commercial manufacturing (23). cGMP will be further described in our next instalment.
Analytical and Bioanalytical Chemists Supporting GLP Studies
Table 3 lists a nonclinical study’s GLP elements divided into five broad categories: Resources, Practices, Analytical and Bioanalytical Testing, Protocol and Study, and Reporting of Study Events. We will provide examples of practice and testing elements relevant to chemists in this section.
Good documentation practice (GDocP) is a core element of GLP compliance (24). Pharmaceutical companies establish their own GDocP aligned with industry standards. For example, the acronym “ALCOA+” is often used to describe components of GDocP: Attributable, Legible, Contemporaneous, Original, and Accurate, along with Complete, Consistent, Enduring, and Available. For the chemist, this means using an electronic lab notebook or ELN to contemporaneously record reagents, solvents, samples, balances, weights, pipettes, and equipment used to prepare and analyze the test and control articles. The analyst must document the technical procedures and data analysis techniques, including the chromatography data system (CDS) processing method and integration parameters. All raw data and corresponding GLP documentation must be retained and archived as per SOPs.
Chain of custody is essential to maintaining the integrity of the GLP study, so there must be documentation of the delivery, receipt, storage, preparation, analysis, and disposition of test and control articles. The study director or test facility manager typically enforces these regulatory aspects. The quality assurance unit (QAU) may conduct an in-study inspection of the analytical chemist preparing test and control article samples to assure correct procedures are followed.
We highlight two specific roles for the analytical chemist working in the lab—the analytical chemist responsible for characterizing the GLP test article and monitoring its stability (21 CFR Part 58.105[a] and [b]); and the bioanalytical chemist responsible for the analysis of blood, plasma, serum, other bodily fluids, or tissues after administration of the test article to the test systems (21 CFR Part 58.120 [4,22], Part 58.130[a] and [c]). Both roles are essential in supporting GLP studies.
Analytical Chemists:
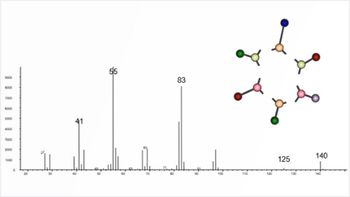
Analytical chemists support GLP studies by developing methods to characterize test articles (drug substances and early-phase drug product formulations) to determine identity, strength, purity, composition, or other characteristics that appropriately define it (2,4). Test articles in GLP studies should be characterized and documented using GLP-compliant methods and procedures (21). The chemist uses phase-appropriate method validation for GLP studies (3,21), as there is often little data available on degradation products and pathways at this early stage of development. In addition, a toxicology study is often conducted using simple formulations or carriers before a final drug product formulation is fully established. High performance liquid chromatography (HPLC) with ultraviolet (UV) detection is commonly used for testing small molecule test articles. The equipment must have proper qualification documentation for a GLP study (7).
Stability of the test and control articles (such as drug substance and dosing solution when applicable) must be established to assign appropriate storage conditions and assure that the concentration of the test article does not change outside of established ranges from the date of manufacture through the end of the study.
Bioanalytical Chemists:
Bioanalytical methods employed in GLP studies are validated in accordance with International Council for Harmonisation (ICH) M10 (25). The guidance applies to bioanalytical methods used to measure concentrations of chemical and biological drug(s) and their metabolite(s) obtained in nonclinical TK studies, nonclinical PK studies conducted as surrogates for clinical studies, and all phases of clinical samples.
Bioanalytical chemists may use techniques such as LC–mass spectrometry (MS), enzyme-linked immunosorbent assay (ELISA), electrochemiluminescence, or surface plasmon resonance to measure the concentration of drug and metabolite in a particular biological matrix such as whole blood, serum, or plasma (26,27).
Core bioanalytical assay validation typically consists of evaluations of the method’s precision, accuracy, selectivity, and specificity. Additional validation experiments are performed to characterize the assay and evaluate the stability of the analyte in the appropriate biological matrix. For example, selectivity must be evaluated in relevant patient populations, presenting a challenge for projects with rare disease indications (26). Stability in the biological matrix is determined over an appropriate concentration range for the assay being validated. Typically, stability is evaluated at room temperature, frozen, and after multiple freeze-and-thaw cycles (25). It is also sometimes necessary to evaluate the assay’s performance in the presence of co-administered medications or elevated levels of the endogenous target (26).
GLP bioanalytical support of large molecule clinical studies also includes immunogenicity testing (28,29). Immunogenicity is the tendency of a drug candidate to elicit an immune response to itself, resulting in the possibility of altered PK or potential adverse clinical events. Immunogenicity testing typically consists of screening, confirmatory, titration, and neutralization assays to identify and characterize the immune response fully (30).
Conclusions and Summary
Analytical chemists are essential in determining the concentration, homogeneity, and stability of test articles and reference articles for nonclinical studies. Bioanalytical chemists are essential in analyzing specimens from nonclinical test systems and clinical test subjects. Compliance with GLP ensures the reliability and integrity of these studies and the accuracy of the data submitted to regulatory authorities.
Disclaimer
This paper provides a high-level overview of GLP regulations and related standards for pharmaceutical scientists in nonclinical and clinical studies. While the goal of the regulation is straightforward, compliance activities are diversified and variable, driven by the company’s SOPs, resources, and compliance culture. The information presented here stems from health regulations, guidance documents, and the authors’ experience. Presenting a concise overview of this complex topic is challenging. The reader is referred to cited references and the company’s internal SOPs for more definitive compliance activities in the laboratory.
Acknowledgements
The authors thank the reviewers for providing timely technical and editorial inputs to this article: Kirk Smith of Smith & Co. Consulting, Alice Krumenaker of Hovione, Mike Shifflet from Kenvue, Doug McDowell of Eurofins Biopharm Products Testing, Kate Evans of Longboard Scientific Consulting, Bob McDowall of McDowall Consulting, David VanMeter of Sartorius, Michael Swartz of Karuna Therapeutics, Chris Tudan of Veloxity Labs, Aimin Tan of Nucro-Technics, and He Meng of Sanofi.
References
(1) Hill, R. G.; Rang H. P. (Eds). Drug Discovery and Development: Technology in Transition, 2nd ed.; Elsevier, 2012.
(2) Dong, M. W. Drug Development Process: Nonclinical Development of Small Molecule Drugs. LCGC North Am. 2022, 40 (10), 484–492. DOI:
(3) Doneski, L.; Dong, M. W. Pharmaceutical Regulations: An Overview for the Analytical Chemist. LCGC North Am. 2023, 41 (6), 211–215. DOI:
(4) CFR Title 21, 58, Good Laboratory Practice for Nonclinical Laboratory Studies (Government Printing Office, Washington, DC, USA)
(5) FDA, Nonclinical Safety Studies for the Conduct of Human Clinical Trials and Market Authorization for Pharmaceuticals (CDER, 2019).
(6) Allport-Settle, M. J. Good Clinical Practice: Pharmaceutical, Biologics, and Medical Device Regulations and Guidance Documents Concise Reference, Vol. 2, Guidance; PharmaLogika, 2010.
(7) Bunn, G. P. (Ed.) Good Laboratory Practice for Nonclinical Studies (Drugs and the Pharmaceutical Sciences), 1st ed; CRC Press, 2022.
(8) OECD Principles of Good Laboratory Practice, Environment Directorate Organization for Economic Cooperation and Development, 1998. DOI:
(9) Whalen, K. Lippincott Illustrated Reviews: Pharmacology, 7th ed; Walters Kluwer, 2018.
(10) Beringer, P. Winter’s Basic Clinical Pharmacokinetics, 6th ed; Lippincott Williams & Wilkens, 2017.
(11) Klassen, C.; Watkins, J. Casarett & Doull’s Essentials of Toxicology, 4th ed; McGraw Hill, 2021.
(12) Kolman, J.; Meng, P.; Scott, G. (Ed.) Good Clinical Practice: Standard Operating Procedures for Clinical Researchers; Wiley, 2021.
(13) ICH, E6 (R3) Good Clinical Practice (GCP) (2021).
(14) Ezzelle, J.; Rodriguez-Chavez, I. R.; Darden, J. M.; et al. Guidelines on Good Clinical Laboratory Practice (GCLP): Bridging Operations Between Research and Clinical Research Laboratories. J. Pharm Biomed Anal. 2008, 46 (1), 18–29. DOI:
(15) Good Clinical Laboratory Practice, World Health Organization.
(16) CFR Title 40, 160, Good Laboratory Practice Standards (Government Printing Office, Washington, DC)
(17) Directive 2004/9/EC of the European Parliament and the Council of 11 February 2004 on the Inspection and Verification of Good Laboratory Practice (GLP) (February 2004).
(18) Directive 2004/10/EC of the European Parliament and of the Council of 11 February 2004 on the Harmonization of Laws, Regulations, and Administrative Provisions Relating to the Application of the Principles of Good Laboratory Practice and the Verification of Their Applications for Tests on Chemical Substances (February 2004).
(19) Huntsinger, D. W. OECD and USA GLP Applications. Ann. Ist Super. Sanita. 2008, 44 (4), 403–406.
(20) Chen, Z. Good Laboratory Practice (GLP) 101–Regulations and Basic Studies (CDER, July 2022).
(21) Tahl, K.; Brown, J. G. Principles of Good Laboratory Practice and Nonclinical Development in Fundamentals of Pharmaceutical and Biologics Regulations: A Global Perspective. Regulatory Affairs Professionals Soc. 2023, 29–36.
(22) Andola, H.; Purohit, V. K., Good Laboratory Practice Requirements: An Overview. N. Y. Sci. J. 2010, 3 (9), 86–90.
(23) CFR Title 21, 210 and 211, Current Good Manufacturing Practice for Finished Pharmaceuticals (Government Printing Office, Washington, DC, USA)
(24) WHO, TRS 966 - Annex 5: WHO Good Data and Record Management Practices. Annex 5, WHO Technical Report Series 966 (World Health Organization, 2016).
(25) ICH, M10 Bioanalytical Method Validation and Study Sample Analysis (2022).
(26) Stevenson, L.; Kelley, M.; Gorovits, B.; et al.. Large Molecule Specific Assay Operation: Recommendation for Best Practices and Harmonization from the Global Bioanalysis Consortium Harmonization Team. AAPS J. 2014, 16, 83–88. DOI:
(27) Vandivort, T. Pharmacokinetic and Toxicokinetic Studies in Fundamentals of Pharmaceutical and Biologics Regulations: A Global Perspective. Regulatory Affairs Professionals Soc. 2023, 53–62.
(28) Williams, K.; Erickson, R.; Fischer, S. K. Overcoming Disease-Specific Matrix Effect in a Clinical Pharmacokinetic Assay Using Microfluidic Immunoassay Technology. Bioanalysis 2017, 9 (16), 1207–1211. DOI:
(29) Law, W. S.; Genin, J. C.; Miess, C.; et al. Use of Generic LC–MS/MS Assays to Characterize Atypical PK Profile of a Biotherapeutic Monoclonal Antibody. Bioanalysis 2014, 6 (23), 3225–3235. DOI:
(30) FDA, Immunogenicity Testing of Therapeutic Protein Products — Developing and Validating Assays for Anti-Drug Antibody Detection (CDER, 2019).
ABOUT THE CO-AUTHORS
Leon Doneski is the director of regulatory CMC for Arcutis Biotherapeutics.
David Roos is a principal scientist at Boehringer Ingelheim Pharmaceuticals.
ABOUT THE COLUMN EDITOR
Michael W. Dong is a principal of MWD Consulting. Direct correspondence to
Articles in this issue
over 2 years ago
Trends in Sample Preparation, Part 1: Current State of the Fieldover 2 years ago
Determining PFAS in Fast Food Packagingover 2 years ago
The Green Analytical Chemistry Workshop (1st TGAC)Newsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.