- March 2022
- Volume 40
- Issue 3
- Pages: 130–135
A Suitable Therapeutic Drug Monitoring Method for Amoxicillin in Plasma by High Performance Liquid Chromatography–UV (HPLC–UV) in Neonates
This simple, rapid, and accurate HPLC-UV method can facilitate routine therapeutic drug monitoring in neonates.
Amoxicillin, a broad-spectrum β-lactam antibiotic, is widely used for treatment of neonatal infections. Despite the unmet need in neonates, an adapted analytical method is still missing in clinical practice. The purpose of this study was to develop and test an easy and credible high performance liquid chromatography–UV (HPLC–UV) method to determine amoxicillin in small volumes of human plasma and use it in routine therapeutic drug monitoring (TDM) of neonates. After a protein precipitation, amoxicillin for standards, quality control samples, and patient samples were separated by LC and measured by UV detection, and tinidazole was used as the internal standard. The calibration range was 0.50–20.0 μg/mL. Intra- and inter-day precisions were less than 4.7%. The acceptance criteria of accuracy (between 85–115%) were met in all cases. A plasma volume of 50 μL was required to achieve the limit of quantification of 0.50 μg/mL. Thus, a simple, rapid, and accurate HPLC–UV method has been developed to detect the concentration of amoxicillin in human plasma. This method was adapted to do TDM of amoxicillin in neonates.
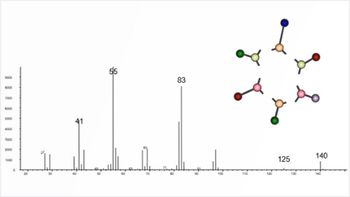
Amoxicillin (C16H19N3O5S, Figure 1) is one of the most commonly prescribed antimicrobial drugs in the world (1,2). Amoxicillin is prescribed for various infections including nose, ear, throat, and skin infections, gonorrhea, genitourinary tract, acute uncomplicated anogenital and urethral infections, and lower respiratory tract infections (3), and it is widely utilized for treating neonatal infections. Amoxicillin is stable in acidic medium and designed for oral use. However, amoxicillin is most commonly administered intravenously (4). It diffuses easily into most of the body fluids and tissues. It also shows low protein binding ability and is principally excreted through glomerular filtration (3).
The pharmacokinetics of amoxicillin showed large variability in neonates (4,5). It is well known that the efficacy of amoxicillin is related to the duration of drug concentrations above the minimum inhibitory concentration (MIC) value (6). Underdosing will speed up bacterial resistance, and overdosing can cause adverse side effects, such as an increase in muscle and liver enzymes, seizures, renal dysfunction, and diarrhea (7). Therefore, therapeutic drug monitoring (TDM) of amoxicillin is required to optimize antimicrobial agents in neonates. An adapted method is a requisition for neonatal TDM practice. Various bioanalytical methods have been reported to measure amoxicillin concentration, consisting of high performance liquid chromatography (HPLC) paired with UV (8–12), fluorescence (13–15), or mass spectrometry (MS) (16,17). Nevertheless, most of these methods have limitations in neonatal clinical practice. The lower limits of quantification (LLOQ) in some of these studies were very low (0.2–1 mg/L), but the volume of the samples were more than 100 μL (9–15). One study on this subject used less volume of samples (40 μL); however, the quantification limit was high (8 mg/L) (8). Other reported studies used either comparatively complicated sample preparation methods (8,9) or utilized expensive methods (16,17). The purpose of the study was to build and test an easy and credible HPLC–UV method to determine amoxicillin in small volumes of human plasma and use it in the routine therapeutic drug monitoring in neonates.
Methodology
Chemicals
Analytical or HPLC grade chemicals and reagents were used. Amoxicillin reference standards and tinidazole (internal standard) were obtained from the National Institute for Drug and Food Control. HPLC-level solvent methanol was procured from Merck Serono. Potassium dihydrogen phosphate (KH2PO4) was obtained from a reagent company named Sinopharm. Sodium hydroxide was purchased from the Dalu chemical reagent factory. For HPLC mobile phase filtration, HV membrane filters (0.45 μm in size) were purchased from the Xianan biochemical instruments factory. A Milli-Q water purification system for ultrapure water was purchased from Millipore. Drug-free human plasma was procured from healthy subjects.
Quality Control Samples and Standards Preparation
The amoxicillin stock solution (0.86 mg/mL) was prepared in solution A (6.8 g/L concentrated KH2PO4 buffer, pH 5.0) and divided into 1 mL aliquots before being stored at a temperature of −70 °C. After that, calibration standards of amoxicillin (0.5, 0.7, 2, 4, 8, 16, and 20 μg/mL) were prepared in plasma. Quality control (QC) samples (low QC: 1.0 μg/mL; medium QC: 10.0 μg/mL; and high QC: 17.5 μg/mL) were equipped by adding proper quantity of the main solution to blank plasma. All the QC samples were split into 50 μL aliquots and conserved at −70 °C. The 19.3 μg/mL tinidazole working solution was saved in water, then split into 1.0 mL aliquots and conserved at −70 °C.
Sample Preparation
According to the procedure, 200 μL of methanol and 20 μL of the internal standard working solution were added into a 50 μL sample of plasma to prepare samples. Next, the samples were vortexed for 1 min, trembled and separated at 4000 rpm at 4 °C by using a shaker, and centrifuged for 10 min, respectively. Then, 100 μL of the supernatant was put into an autosampler vial with an insert and diluted with 100 μL of water. Finally, 20 μL of sample volume was analyzed in the LC–UV system via the injector.
Instruments and Chromatography
For the HPLC–UV method, a Waters 2695 separations module and a Waters 2487 UV detector were used. For the chromatographic separation, an InertSustain column (RP-18e, 250 mm × 4.6 mm) from Shimadzu was used. The wavelength was set at 230 nm. The gradient of the mobile phase was solution A (6.8 g/L concentrated buffer of KH2PO4 potassium with added sodium hydroxide, pH 5.0), and the B solution contained methanol. Mobile-phase composition was linearly altered for 15 min from 96% A to 50% A. The procedure was then returned to 96% A at 16 min and kept until 21 min, while being pumped with a constant flow rate of 1.5 mL/min. The mobile phase was arranged every day accordingly, degassed by ultrasonication prior to use, and prohibited from recirculating during the procedure.
Method Validation
The method was validated according to the guidelines of the bioanalytical procedure approved by the Food and Drug Administration (FDA) (18) and the European Medicines Agency (EMA) (19). The terms for validation contained selectivity, linearity, LLOQ, matrix effect, accuracy, precision, recovery, and stability.
Selectivity
To assess the selectivity of the method, six different blank plasma samples were analyzed. The method selectivity was defined as the lack of disturbance at the retention times of amoxicillin, the internal standard from the blank plasma components, and the lack of cross-interference among them using the propositioned extraction technique and LC–UV conditions.
Linearity
Fresh preparations were used for three days to determine the linearity of the method. Amoxicillin calibration curves were produced by spiking the sample of matrix with a concentration range 0.5–20 μg/mL. The calibration data linear regression analysis was performed by using the equation: y = a + b·C, where y is the peak area ratio of amoxicillin to internal standard, C is the nominal amoxicillin concentration in calibration samples, and a and b are the intercept and the slope of the curve, respectively.
For each calibration curve, the slope, intercept, and correlation coefficient (r2) were calculated. The calibration curve was tested: a) the mean value should be within ±15% of the theoretical value (LLOQ within ±20%), and b) the precision around the mean value should not exceed a 15% coefficient of variation (CV) (LLOQ within ±20%).
Lower Limit of Quantification (LLOQ)
The LLOQ was ascertained as the signal-to-noise (S/N) ratio being greater than five. The analyte peak should be identifiable, discrete, and reproducible with an accuracy of 80–120%, and a precision of 20%.
Matrix Effect
The potential interference of the matrix compounds in the quantification of amoxicillin was evaluated. A spiked blank plasma sample and a working standard solution were investigated at the LLOQ level.
Accuracy, Precision, and Recovery
Precision, accuracy, and recovery were evaluated at three concentrations (QC1, 1.0 μg/mL; QC2, 10.0 μg/mL; and QC3, 17.5 μg/mL). The intra- and inter-day accuracies were shown using an equation: [(measured concentration/theoretical concentration) × 100]. Intra-day assay accuracy and precision were computed using five replicates during every analytical procedure. Inter-day assay accuracy and precision were reported by evaluating the three QCs on three different days. The precision had to remain under 15%, and the bias range must be within 85–115%. The recovery of the method was evaluated by the responses of the three extracted concentrations compared with the nonextracted standards (equivalent to 100% recovery).
Stability
To assess the stability of the samples during the sample treatment process, the stability procedures were defined. For QC1 and QC3, short stability was established and assessed by comparing assay values in triplicate at room temperature after 6 hr.
By performing assaying of the QC1 and QC3 freeze-thaw, stability was assessed in triplicate over three freeze–thawing cycles (stored at −70 °C for 24 hr, thawed at room temperature, and refrozen for 24 hr constitutes one cycle). The measured concentrations were then compared to the nominal value.
Post-preparative stability was established by determining the QC1, QC2, and QC3 in an autosampler at 4 °C by injecting extracts immediately after the pretreatment, then re-injecting after 72 hr.
To establish long-term stability, samples stored at −70 °C over 50 days were analyzed.
Application in Therapeutic Drug Monitoring (TDM)
The developed method was routinely implicated in TDM of amoxicillin in neonates. This study was conducted according to the guidelines of the Declaration of Helsinki and with the approval by the local research ethics committee. For this study, 97 neonates receiving amoxicillin as part of their antimicrobial treatment were used. The standard dosing regimen was 30 mg/kg twice daily. The trough concentrations at steady-state (one day after the start of therapy) were drawn according to standard clinical practice. Using EDTA tubes, all the blood samples were collected and centrifuged for 10 min at 4000 rpm at 4 °C to segregate the components of plasma. Then, the plasma fraction was shifted to a new tube and stored at −70 °C until analysis. All samples were determined in a month.
Results
Selectivity
The chromatograms of the blank plasma and LLOQ are shown in Figure 2a and 2b, respectively. No interferences were detected at the retention times of amoxicillin and tinidazole.
Linearity
The calibration curves were linear over the concentration range of 0.5–20 μg/ mL in human plasma. The following equation was obtained: y = 0.0477x + 0.0003 (r2 = 0.9948). The average values of calibration concentrations were within 97.7–105.2% of the theoretical values. Other than the LLOQ, bias was within the range of 83.5–102.7% and the precision was 8.8%.
Lower Limit of Quantification (LLOQ)
The lower limit of quantification was 0.5 μg/mL.
Matrix Effect
The peak areas were evaluated as being similar enough in a way that the matrix effect can be judged insignificant.
Accuracy, Precision and Recovery
Intra- and inter-day precision and accuracy are shown in the Table I. Overall, intra-day precision was lower than 4.74%, while inter-day precision was lower than 4.30%. In all cases, the acceptance criteria of accuracy (range, 85 and 115%) were met. Amoxicillin recovery was 107.1 ± 10.7% (range was 94.8–114.7%).
Stability
Short-term stability was shown that the QC samples were stable for 6 hr stored at room temperature (biases range, −14.3 and 8.7%). Freeze thawing three consecutive cycles showed no signifi- cant degradation for amoxicillin (biases range, 14.8 to −5.0%). In autosampler, the extracted samples were stable for approximately 72 hrs at −4 °C (biases range, −14.9 to 3.4%). From the literature, in case of long-term stability the samples were stable for over 50 days stored at −70 °C, the concentrations of the samples have no significant degradation (deviation <2.03%) (15), which indicated that the samples in this study were stable (measured in a month).
Therapeutic Drug Monitoring (TDM)
A total of 97 neonates were included with a median gestational age (GA) of 37.86 weeks (the range was 28.29–41.29 weeks), a median postnatal age (PNA) of six days (the range was 0–18 days), and current weight (CW) of 2.94 kg (the range was 1.06–4.13 kg). Figure 3 showed an original chromatogram from the analyzed patients’ samples. Figure 4 showed the distribution of trough concentrations. Only 51.5% (n = 50) of neonates had trough concentrations higher than 2 μg/mL.
Discussion
Because of the unique features in neonates, the analytical method ought to be well adapted and find a balance between small sample volume and high sensitivity. After reviewing previously published methods to determine the amoxicillin concentration, most of these methods have limitations in neonatal TDM, such as cumbersome sample preparation, a large number of plasma samples, a high LLOQ, and an expensive cost. In this study, all of these common problems were resolved. The required plasma volume was approximately 50 μL, which was suitable for neonatal physiological condition, and the LLOQ was only 0.5 μg/mL. At the same time, the sample preparation process was significantly simplified. In addition, the HPLC–UV instrumentation is common in hospitals, so this method is easy to generalize. Obviously, these improvements allow to better interpret TDM results in neonates.
Amoxicillin is not stable in plasma at room temperature as its β-lactam ring is more susceptible to hydrolytic degradation by plasma amidase (20). Considering the water solubility of amoxicillin and its chemical stability, along with the viscosity of the solution (risk of operational error), methanol and water (1:1) were used as the diluent during the solution preparation.
This developed method was further evaluated in neonatal TDM practice. As shown in the results, the trough concentrations were highly variable. As a time-dependent, anti-infective drug, amoxicillin efficacy correlates with the time of drug concentration above the MIC (21). According to the breakpoint tables for interpretation of MICs and zone diameters (22), the MIC breakpoints were 0.5 μg/mL for Viridans streptococci and Gram-negative anaerobes, 1.0 μg/mL for Pasteurella multocida, 2.0 μg/mL for Haemophilus influenzae, 4.0 μg/mL for Enterococcus spp. and Gram-positive anaerobes (except Clostridium difficile), and 8.0 μg/mL for Enterobacteriaceae. Our study showed that 8.4% (n = 47) of patients had a trough concentration of less than 2 μg/mL, indicating a high risk of treatment failure in these patients. In this situation, a higher dose or other antimicrobial treatment ought to be suggested to these patients. Therefore, TDM should be advised to optimize the treatment of amoxicillin in neonates.
Conclusion
A simple, rapid, and accurate HPLC–UV method has been developed to determine the amoxicillin concentration in plasma. The small volume of plasma (50 μL) and sensitive LLOQ (0.5 μg/mL) make it well adapted to neonatal TDM practice. Only 51.5% of neonates had trough concentrations higher than 2 μg/mL, so TDM should be advised to optimize the treatment of amoxicillin in neonates.
Acknowledgments
This work is supported by National Science and Technology Major Projects for Major New Drugs Innovation and Development (2017ZX09304029-002), Young Taishan Scholars Program, and the Young Scholars Program of Shandong University. The authors have no conflicts of interest to declare.
References
(1) T.P. Van Boeckel, S. Gandra, A. Ashok, Q. Caudron, B.T. Grenfell, S.A. Levin, and R. Laxminarayan, Lancet. Infect. Dis. 14(8), 742–750 (2014).
(2) R. Zhang, J. Tang, J. Li, Q. Zheng, D. Liu, Y. Chen, et al., Environ. Pollut. 174, 71–77 (2013).
(3) GlaxoSmithKline, Amoxil (amoxicillin capsules, tablets, chewable tablets, and powder for oral suspension) prescribing information. GlaxoSmithKline, Research Triangle Park, NC (2006).
(4) G.M. Pacifici and K. Allegaert, J. Chemother. 29(1), 57–59 (2017).
(5) A. van Boekholt, H. Fleuren, J. Mouton, C. Kramers, T. Sprong, P. Gerrits, and B. Semmekrot, Eur. J. Clin. Microbiol. Infect. Dis. 35, 1007–1012 (2016).
(6) G.M. Pacifici, J. Labatia, H. Mulla, and I. Choonara, Eur. J. Clin. Pharmacol. 65, 191–198 (2009).
(7) C.L. Shaffer, A.M. Davey, J.L. Ransom, Y.L. Brown, and P. Gal, Ann. Pharmacother. 32, 482–484 (1998).
(8) J. Pullen, L.M. Stolk, C. Neef, and L.J. Zimmermann, Chromatogr 21, 1259–1265 (2007).
(9) B. Buszewski, M. Szultka, P. Olszowy, S. Bocian, T. Ligor, Analyst 136, 2635–2642 (2011).
(10) M.C. Verdier, O. Tribut, P. Tattevin, Y. Le Tulzo, C. Michelet, and D. Bentué-Ferrer, Antimicrob. Agents. Chemother. 55, 4873–4879 (2011).
(11) S.M. Foroutan, A. Zarghi, A. Shafaati, A. Khoddam, and H. Movahed, J. Pharm. Biomed. Anal. 45, 531–534 (2007).
(12) G. Hoizey, D. Lamiable, C. Frances, T. Trenque, M. Kaltenbach, J. Denis, and H. Millart, J. Pharm. Biomed. Anal. 30, 661–666 (2002).
(13) K. Miyazaki, K. Ohtani, K. Sunada, and T. Arita, J. Chromatogr. 276, 478–482 (1983).
(14) H. Mascher and C. Kikuta, J. Chromatogr. 506, 417–421 (1990).
(15) H.J. Mascher and C. Kikuta, J. Chromatogr. A. 812, 221–226 (1998).
(16) X. Dong, L. Ding, X. Cao, L. Jiang, and S. Zhong, Biomed. Chromatogr. 27, 520–526 (2013).
(17) B. Cirić, D. Jandrić, V. Kilibarda, J. Jović- Stosić, V. Dragojević-Simić, and S. Vucinić, Vojnosanit. Pregl. 67, 887–892 (2010).
(18) U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), and Center for Veterinary Medicine (CVM), Bioanalytical Method Validation Guidance for Industry (2018).
(19) European Medicines Agency, Committee for Medicinal Products for Human Use, Guideline on bioanalytical method validation (2012).
(20) J. Concannon, H. Lovitt, M. Ramage, L.H. Tai, C. McDonald, V.B. Sunderland, Am. J. Hosp. Pharm. 43, 3027–3030 (1986).
(21) Den. Van and J.N. Anker, Ther. Drug. Monit. 28, 816 (2006).
(22) European Committee on Antimicrobial Susceptibility Testing, Breakpoint tables for interpretation of MICs and zone diameters (2016).
Xing-Kai Chen is with the Department of Pharmacy at Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School, in Nanjing, China. Hai-Yan Shi, Xin Huang, and Wei Zhao are with the First Affiliated Hospital of Shandong First Medical University, in Jinan, China. Huang Zhao, Wasim Khan, Yi Zheng, and Guo-Xiang Hao are with the School of Pharmaceutical Sciences at Shandong University, in Jinan, China. Chen Kou is with the Beijing Obstetrics and Gynecology Hospital at Capital Medical University, in Beijing, China. Li-Wen Li is with the Intensive Care Unit at the First Affiliated Hospital of Shandong at the First Medical University, in Jinan, China. Direct correspondence to:
Articles in this issue
Newsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.