- LCGC North America-02-01-2005
- Volume 23
- Issue 2
Photodegradation and Photstability Studies of Bendroflumethiazide in Pharmaceutical Formulations and Urine Samples by Micellar Liquid Chromatography
A simple HPLC procedure is described for the determination of bendroflumethiazide (BMFT) in pharmaceutical formulations and urine samples. No interferences from common additives or other drugs frequently administered with BMFT or from endogenous compounds in urine samples were found. The lack of an organic solvent in the mobile phase reduces the risk of environmental contamination and human toxicity.
Bendroflumethiazide (BMFT RS]-3-phenylmethyl-3,4-dihydro-6-trifluoromethyl-2H-1,2,4-benzothiadiazine-7-sulfonamide-1,1-dioxide) is a potent diuretic drug extensively used for the treatment of hypertension and oedema that belongs to the thiazide family (1). BMFT is well absorbed from the gastrointestinal tract after oral administration and the absorption is not affected by food. It lowers blood pressure and removes extra salt and water from the body by acting on the kidneys. BFMT is usually prescribed as tablets and frequently in combination with b-blockers. Because of the increase in urine flow, which reduces body weight, the administration of BFMT is forbidden in sports where the competition is based on weight classes (2). Because of the diluting effect, intake of such drugs could also result in suppression of other doping substances below their limits of detection.
BFMT hydrolyzes to 5-trifluoromethyl-2,4-disufhoamoyl-aniline (TFSA) and phenylacetaldehyde in acidic media at high temperature. Under certain conditions, BFMT has also been reported to produce the thiazide diuretic hydroflumethiazide (HFMT, 3,4-dihydro-6-trifluoromethyl-2H-1,2,4-benzothiadiazine-7-sulfonamide-1,1-dioxide) (3,4). HFMT is formed by the reaction of TFSA with formaldehyde, which is a degradation product of the polymers polyethylene glycol 6000 and poloxamer 188. High humidity promotes this reaction.
Rapid and reliable methods are required for drug monitoring in therapeutic and doping control. Different procedures including amperometric and conductimetric titrimetries (5), polarography (6), capillary electrophoresis (7), electrochromatography (8), and chromatographic techniques, such as thin-layer chromatography with fluorescence scanning (9,10), reversed-phase liquid chromatography (1,3,11,12), and gas chromatography (13,14) with either ultraviolet (UV) or fluorescence detection, have been described to measure BFMT alone or with other compounds. Several authors have also investigated the stability of BFMT and the kinetics of the degradation process in aqueous, methanolic, and polymeric solutions (3,4,15,16). Barnes and Nash have studied the stability of BFMT in capsules (17,18). However, degradation processes in physiological samples (urine, serum, or plasma) and the possibility of photochemical degradation, very common in the group of thiazide diuretics, are rarely mentioned in analytical reports. This may limit their usefulness in the therapeutic monitoring of BFMT at the levels found in patients and also in pharmacokinetic bioequivalence studies.
The comments found in the literature about the adequate medium to prepare BFMT solutions are not convincing. In this work, the experimental conditions needed to prevent the degradation of this diuretic, induced by different pathways, in the analytical laboratory are studied. When a sportsman deliberately takes BFMT, it is possible that the drug remains undetected if adequate precautions are not taken.
A simple, rapid and selective chromatographic procedure that uses a micellar mobile phase of sodium dodecyl sulfate is described and applied to the control of some pharmaceutical formulations and spiked urine samples containing BFMT. The procedure resolves the drug from its major degradation product. Micellar media have been demonstrated to slow down the degradation of diverse drugs in different matrices (19-22). Micellar chromatographic methods have the advantages of the direct injection of samples without any pretreatment other than filtration, and the low toxicity of the employed mobile phases.
Experimental
Reagents:
BFMT and HFMT were supplied from Sigma (St. Louis, Missouri). TFSA was obtained by hydrolysis or by degradation induced by light exposure. The pharmaceuticals Betadipressan, Neatenol Diu and Neatenol Diuvas were purchased in a local pharmacy.
Other reagents were sodium dodecyl sulfate (SDS) (Merck, Darmstadt, Germany), sodium dihydrogenphosphate monohydrate, HCl (Panreac, Barcelona, Spain), sodium hydroxide (Scharlab, Barcelona, Spain), acetic acid (Panreac, Barcelona, Spain,) and methanol (J.T. Baker, The Netherlands). Distilled water was used to prepare the aqueous solutions.
Apparatus and chromatographic conditions: Hydrolysis of BFMT was performed in a thermostatic bath (Model BA-4, Raypa, Terrassa, Spain) at 100 °C. The HPLC system consisted of an Agilent Technologies chromatograph (Series HP 1100, Palo Alto, California), comprising an autosampler with 2-mL vials (Model G1313A), a thermostated column compartment (Model G1316A), and a UV-vis detector (Model G1314A). The signal was acquired with a PC connected to the chromatograph via HP Chemstation software.
The analytical separation was accomplished using a Kromasil C18 reversed-phase column (5 μm particle size, 125 mm à 4.6 mm) connected to a 30-mm guard column of similar characteristics (Scharlab). The flow-rate was 1 mL/min and the injection volume 20 µL. The chromatographic runs were performed at 25 ±0.2 °C. Monitoring was performed at 274 nm. An ultrasonic bath was used to dissolve the standards and pharmaceuticals (Model Ultrasons-H, Selecta, Abrera, Spain).
The micellar mobile phase used in the stability studies was 0.05M SDS-0.01 M monobasic sodium phosphate buffered at pH 3. The same mobile phase was used to analyze the pharmaceutical and urine samples and was filtered though 0.45-μm nylon membranes with a diameter of 47 μm (Micron Separations, Westboro, Massachusetts).
A triple-quadrupole Quattro LC mass spectrometer with an orthogonal Z-spray-electrospray interface (Micromass, Manchester, UK) was used to confirm the identity of the main degradation product. Dry and nebulization were made with nitrogen using a flow of 400 L/h and 80 L/h, respectively. The temperature of the source block was set to 120 °C and the desolvation temperature was 150 °C. A capillary voltage of 3.5 kV was used in the positive or negative scan mode and the cone voltage was set to 30 V. Sample solutions (approx. 5 μg/mL) dissolved in methanol, were infused via syringe pump directly connected to the interface.
Standard solutions and urine samples: Stock standard solutions containing 100 μg/mL of BFMT or HFMT were prepared. The drugs were dissolved in methanol with the aid of an ultrasonic bath and made up to the mark in the volumetric flask with 0.1M SDS buffered at pH 3 or 7 with phosphate. The final content of methanol in the solution was 10% (v/v). For the stability studies, BMFT standard solutions or spiked urine samples with BFMT were diluted to 20 μg/mL with the same SDS solution. For analysis of the pharmaceuticals, several standard solutions were prepared in the 4-20 μg/mL range, and for analysis of the urine samples in the 0.4-90 μg/mL range. All solutions were protected from light (except some used in the stability studies) with aluminum foil to avoid extensive photochemical degradation of the drug. Fresh solutions were prepared periodically.
Table I: Analysis of several formulations containing bendroflumethiazide
Procedure: The pharmaceuticals analyzed were tablets. The average weight per tablet was calculated from 10 units. The tablets were ground and reduced to a homogeneous fine powder in a mortar. Several portions of this powder were accurately weighed and sonicated in the presence of methanol (10% v/v of the final content) in an ultrasonic bath. A 0.1 M SDS solution at pH 3 was added to favor the extraction of the analyte, again using the ultrasonic bath. A dilution was then made with the same micellar solution to a final concentration of 10 μg/mL. The excipients in the tablets were not soluble in the micellar medium, hence the sample solutions were filtered before their injection into the chromatograph. However, the filtration was always performed directly into the autosampler vials through 0.45-μm nylon membranes of 13 mm diameter (Micron Separations).
Table II: Day-to-day calibration parameters obtained for bendroflumethiazide spiked standards protected from light
The urine analyses were performed with 1-mL urine samples, which were diluted 1:25 also with 0.1 M SDS at pH 3 before injection. The standard solutions of BFMT and urine samples spiked with BFMT were also filtered before injection into the chromatograph as explained above. All solutions were protected from light by covering them with aluminium foil to avoid photochemical degradation of the drug. The transparent glass vials were also protected from light.
Results and Discussion
Selection of chromatographic conditions: A micellar solution of 20 μg/mL of BFMT was prepared at pH 3 and protected with aluminium foil to prevent any photochemical degradation. A second micellar solution of the same concentration was also prepared at pH 3, but stored unprotected from light. This solution was used to study the separation of the parent drug from its photodecomposition product. After several hours of exposition to daylight (beside a laboratory window), the vial containing BFMT was kept in the dark with aluminium foil, which partially stopped the degradation process, making the chromatographic analysis possible over several hours.
A micellar mobile phase containing 0.05M SDS at pH 3 was selected to perform the analysis. No organic modifiers were added to the mobile phase. A surfactant concentration above 0.05 M leads the degradation product of BMFT to extremely short retention times, whereas smaller concentrations of SDS would not assure the formation of micelles. BMFT is a basic compound (pKa = 8.5) and the same acid-base species (cationic in this instance) will predominate in the whole working pH of the column used (2.5 < pH < 7.5). The anionic surfactant in the micellar solution increases the stability of the protonated species of the BMFT and consequently their protonation constants (23). As a result, the retention time of the drug will not vary in the pH range of the column. Nevertheless, at pH 7 the degradation process was found to be faster. For these reasons the pH selected to perform the experiments was set to 3. With the selected mobile phase, the retention time of BFMT was 17.5 min (Figure 1a). In the solution exposed to daylight or artificial light, three peaks were observed at 2.5, 2.7, and 17.5 min (Figure 1b).
Figure 1: Chromatograms of two standard solutions of BFMT prepared at pH 3 (a) protected from daylight or (b) exposed to daylight. Mobile phase: 0.05 M SDS-pH 3.
Photodegradation of BFMT in standard solutions: The stability of BFMT solutions was studied at acidic and neutral pH. As BFMT is partially soluble in water, it was dissolved in a small amount of methanol and further diluted with water or SDS 0.1M. The final methanol content was 10%. The group of thiazide diuretics is known to be photochemically unstable although this has rarely been reported in analytical procedures (3,24-26). Thieme and colleagues reported the hydrolysis as the most important reaction that diminishes the stability of these benzothiadiazines (27). To study the kinetics of the degradation process, solutions of BFMT buffered at pH 3 and 7 were protected from light or exposed to standard laboratory lighting (fluorescence light Osram 40 W, Germany) at room temperature. The solutions were chromatographically analyzed to know their degradation degree without preventing contact with air or expelling oxygen from them.
When freshly prepared micellar solutions of BFMT buffered at pH 3 and protected from light are chromatographed, only the peak of BMFT (17.5 min) is observed. However, a small peak appears at 2.7 min after 3 h. Without protection from light, this peak is observed 30 min after preparing the solution. At pH 7, it was found that BFMT decomposed faster. The area of the peak of BFMT protected from light at pH 3 decreased by 0.1% after 3 h and by 1% after 30 h. These ratios were 1% and 17.1% for the solutions at pH 7 protected from light at the same times. In Figure 2, some of the chromatograms obtained in different conditions are shown.
Figure 2: Chromatograms of two standard solutions of BFMT protected from light at (a) pH 3 and (b) pH 7 injected 30 h after its preparation. Mobile phase: 0.05 M SDS-pH 3.
The logarithms of the difference between the area at any time At and the final area of the chromatographic peak, Aâ (= 0), were plotted against time in Figure 3 for diverse conditions. The curves of decomposition were found to obey a first-order kinetics according to Equation 1 with correlation coefficients higher than 0.99 in all instances:
where A0 is the area at time zero and k1 is the apparent first-order constant. The solutions protected from light and buffered at pH 3 (Figure 3a, line 1) were stable during long periods, except those buffered at pH 7, which had a half-life of six days (Figure 3a, line 3). The solutions unprotected at pH 3 (Figure 3a, line 2) suffered photodegradation with a half-life of 40 days. The degradation process is then catalyzed by light exposure and pH, being faster as the pH and time exposure increase.
Photodegradation of BFMT in urine samples: As the degradation process is slower at pH 3, the stability of BFMT in urine samples was studied under these conditions. The direct injection of a large number of urine samples can shorten the life of the chromatographic column or can force frequent regeneration of the stationary phase. For this reason, the dilution of urine samples is convenient, although the injection of undiluted samples to reach lower limits of detection is feasible.
Spiked urine samples were prepared by mixing one volume of urine and 25 volumes of a solution of the drug buffered at pH 3 and kept from light or exposed to standard laboratory lighting at room temperature. No precautions were taken to prevent contact of the samples with air. The kinetics of the degradation was also studied. The logarithm (At - Aâ) was also plotted versus time (Figure 3b) for spiked urine samples kept or exposed to light. The apparent first-rate constants were obtained from the slopes of the linear segment according to Equation 1. The solution protected from light was stable for at least 48 h (Figure 3b, line 1). After two days, the area of the peak of BFMT decreased by 1%, whereas that unprotected (Figure 3b, line 2) suffered a faster photodegradation: it decreased by 2% after 1 h.
Figure 3: First-order plots for the degradation of BFMT in SDS media at (a) pH 3 protected from light (line 1), exposed to artificial light (line 2), or prepared at pH 7 protected from light (line 3); and (b) in a urine matrix at pH 3 protected from light (line 1) or exposed to artificial light (line 2). All the solutions were prepared in 0.1 M SDS.
Chromatographic study of the degradation products of BFMT: In the literature, 5-trifluoromethyl-2-4 disulfoamoyl-aniline (TFSA) is reported as the main degradation product of BFMT hydrolysis (3,4). Although rarely, a rapid hydrolysis of this drug under light exposure has been mentioned (3). The diuretic HFMT has been reported to form by the reaction of the hydrolysis product, TFSA, with formaldehyde in solid dispersions of BFMT in polymers (4).
Under the experimental chromatographic conditions used in this work, when a solution of BFMT protected from light at pH 3 is injected, a peak is observed at 17.5 min and after several hours a second peak is found at 2.7 min. If the solution is exposed to daylight or artificial light, a third peak is found at 2.5 min. The peak at 17.5 min was assumed to correspond to BFMT, as this was the retention time obtained for the standard solution. However, the identity of the peaks at 2.5 and 2.7 min was subject to controversy. Standard solutions of the degradation product HFMT prepared at pH 3 and protected from light were investigated. This product eluted at 2.9 min and did not seem to correspond to either of these peaks. However, the lack of a standard for TFSA did not allow the identity of the peaks at 2.5 and 2.7 min to be assured.
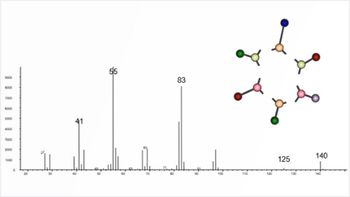
In order to assign the identity of the photochemical products of BFMT, two standard solutions of the diuretic protected and exposed to light for several hours after their preparation were analyzed in a triple- quadrupole mass spectrometer. These solutions were prepared in methanol as the use of micellar media in a mass spectrometer is problematic because of the high concentrations of surfactant that are usually employed. The mass spectrometry (MS) analyses of both samples in the negative mode showed two signals that were identified as the diuretic BFMT (m/z = 420, molecular weight of the compound minus one hydrogen) and its degradation product TFSA (m/z = 318). No other signals for the solution protected from light were obtained. However, an additional signal appeared in the solution exposed to light at m/z = 286. This signal corresponds to a derivative of TFSA formed by oxidation of sulfide side-chain substituents to sulfoxide (R-SO2-R ? R-SO-R). Thieme and colleagues also observed this oxidation process in several thiazide diuretics (27). Consequently, the peak observed at 2.7 min in the chromatograms was assumed to correspond to TFSA and the peak at 2.5 min to the sulfoxide derivative of TFSA. The same compounds were identified in the negative mode.
In a parallel study, a solution of BFMT in a strong acidic medium was heated at 100 °C during 1 h in the dark to avoid photodegradation. Acetic acid was used instead of hydrochloric acid because of the interference of the chloride ions in the MS analysis. The surfactant was not added because it decomposes at high temperature. Aliquots of this solution were taken and cooled rapidly to stop the reaction. The pH of the solution was increased by dilution with 0.1 M SDS at pH 3, previously to the injection in the chromatographic system. Under these conditions, two peaks were observed again at 2.7 and 17.4 min. Aliquots diluted with water were also analyzed by MS, which showed that these peaks corresponded to BFMT and TFSA. No chromatographic peaks or MS signals were obtained that could indicate the presence of HFMT formed under light exposure or acid hydrolysis in the experimental conditions used in this work.
Analysis of Pharmaceutical Formulations and Urine Samples
Pharmaceutical formulations:
The study above indicates that solutions of BFMT are more stable at pH 3 protected from light. The control of BFMT in pharmaceutical formulations was performed over solutions prepared in these conditions, which assured the integrity of the compound for at least two days. The same mobile phase used in the stability studies (0.05 M SDS at pH 3) was employed for the analysis of the pharmaceuticals. This mobile phase allows the formation of the photodegradation product to be easily controlled.
Three pharmaceuticals containing BFMT usually prescribed in our country were analyzed (Table I). Calibration curves were built using the areas of the chromatographic peaks from triplicate injections of standards at five increasing concentrations in the range 4-20 μg/mL. To study the variability of the calibration parameter, the curves were obtained in three consecutive days (same set of BFMT standard) or in different days over two months (different sets of BFMT standards). Standard solutions were prepared periodically and protected from light. The parameters of the fitted straight lines are given in Table II. Coefficients of regression were always r > 0.999 and the slope values were similar among them. The accuracy and precision of the analysis were evaluated in assays performed during the same day and consecutive days. The values shown in Table III correspond to within-day and day-to-day analyses of an aqueous solution containing 10.2 μg/mL of BFMT. This unique solution was injected on three consecutive days. Table III also shows the results obtained for different solutions of the same concentration injected over two months. The low variability and high precision of the results are evident.
Table III: Inter- and intraday accuracy and precision obtained for standards of bendroflumethiazide protected from light
Ten samples of each pharmaceutical formulation were analyzed making triplicate injections to obtain average values of the drug concentration. For this purpose, an appropriate amount of each sample was weighed to prepare solutions containing approximately 10 μg/mL of the drug. Table I gives the declared and found contents, together with the label claim percentages, which were in the 97-100% range. The excipients were eluted with the dead time or did not absorb at the measuring wavelength. The compounds administered in combination with BFMT, atenolol, and hydralazine yielded chromatographic peaks at 38 and 42.9 min, respectively, and did not interfere in the analyses. The peak of propranolol overlapped with that of hydralazine. Figure 4 depicts the chromatograms of the three pharmaceuticals analyzed in this work.
Figure 4: Chromatograms of several formulations containing BFMT: (a) Neatenol Diu, (b) Neatenol Diuvas, and (c) Betadipresan. BFMT 5 bendroflumethiazide, ATL 5 atenolol, HDL 5 hydralazine and PPL 5 propranolol. Mobile phase: 0.05 M SDS-pH 3.
Urine samples: The analytical figures of merit were obtained using drug-free urine samples collected from healthy adult volunteers (men and women). The matrix and spiked urine samples were analyzed using the mobile phase of 0.05 M SDS at pH 3. No interference from the proteins and endogenous components of the urine was observed with the peak of BMFT (Figure 5). It was possible to observe the peak of TFSA, but partially overlapped with the urine matrix. This is not critical to guarantee the quantification of the parent drug.
Figure 5: Chromatograms of (a) a blank urine sample and (b) a spiked urine sample with BFMT protected from light (1 mg/mL). See Figure 1 for peak identification. Mobile phase: 0.05 M SDS at pH 3. The samples were diluted with 0.1 M SDS at pH 3.
The precision of the procedure was evaluated using a urine matrix spiked with six different known concentrations of the drug. The same set of spiked samples were analyzed on the same day and on different days up to six days later to determine the variability (Table IV). The day-to-day precision was <1.4%. Each level of concentration was injected 10-fold every day. This analysis was also performed using different solutions of the same concentration injected for a period of two months (Table V). The low variability and high precision values of the assays indicate the usefulness of the method.
Table IV: Inter- and intraday precision obtained for the same spiked urine standards of bendroflumethiazide protected from light and injected over three consecutive days
The same BFMT standards at seven increasing concentrations in the range 1-90 μg/mL were injected during three days to obtain the variability of the parameters of the calibration curve (Table VI). The curves were constructed using the measured areas of the chromatographic peaks of 10 injections. The results in Table VI show a good linearity (r > 0.9999) over the studied concentration range and a relative standard deviation (RSD) of the slopes < 4%. The calibration standards can be used during three days without observing important degradation. Three calibration curves were further constructed using different BFMT standards at seven concentrations in the same range 1-90 μg/mL to determine the variability of the intercepts and slopes between independent calibration curves. The results, also shown in Table VI, indicate the small day-to-day variability of the slopes. The slopes are very similar to those obtained in the micellar matrix (Table II), indicating the goodness of the procedure. The limit of quantification of BFMT in urine solutions, defined according to 10-s criteria, was 0.33 μg/mL.
Table V: Inter- and intraday precision obtained for different spike urine standards of bendroflumethiazide protected from light and injected over several days.
To determine the reliability of the assay, 15 urine samples from different volunteers were used. The matrix samples (in the absence of BFMT) were chromatographed using the proposed procedure. Chromatograms were inspected for the presence of interfering peaks from endogenous compounds. No interference was found with the peak of BFMT.
Table VI: Day-to-day calibration parameters obtained for bendroflumethiazide spiked urine samples protected from light
Finally, the procedure was applied in a pharmacokinetic study to demonstrate its usefulness. The pharmacokinetics of thiazide diuretics have been studied less extensively than those of loop diuretics. Some thiazide diuretics are metabolized primarily by the liver (for example, bendroflumethiazide, polythiazide and indapamide) while others are primarily excreted unchanged in the urine (for example, chlorothiazide, chlor- thalidone, hydrochlorothiazide, hydroflu-methiazide and trichlormethiazide). The reported half-life of BFMT is 2-5 h (28). BFMT has also been reported to be completely absorbed from the gastrointestinal tract, and there are indications that it is fairly extensively metabolized. About 30% is excreted unchanged in the urine.
A urinary excretion study was performed with a healthy volunteer who ingested a 5-mg BFMT tablet of Neatenol Diu formulation. A sample was collected just before the administration of the drug to be used as blank. Other urine samples were collected at appropriate time intervals post-dose, protected from light and refrigerated at 4 °C until analyzed. Figure 6 shows the urine concentration profile of BMFT. The dose excreted unchanged for BMFT was 1.28 mg (25.6%), which makes sense to the results reported in the literature. The peak of TFSA was observed 12 h after the ingestion of the drug. BMFT could be detected up to 24 h from its ingestion.
Figure 6: Urine concentration profile of BMFT after oral administration of a 5 mg tablet formulation to a healthy volunteer.
Conclusions
The studies performed in this work have shown that BFMT solutions are stable at pH 3 when protected from light for at least 48 h. The degradation seems to be slightly slower in urine matrices as it is indicated by the higher slope of the degradation curve. The degradation is catalyzed by light exposure and pH, being faster as the pH and time exposure increase. BFMT is completely resolved from its major degradation product (TFSA) using a mobile phase of 0.05M SDS at pH 3. When the solution of BFMT is directly exposed to the lighting, TFSA suffers and oxidation process, originating a second degradation product, which is also chromatographically detected using the procedure developed.
The chromatographic procedure can be applied to control the decomposition degree of standards and pharmaceuticals during the analysis, or the quality of pharmaceuticals, and also for the doping control in urine samples. It shows good accuracy, repeatability and selectivity either to determine BFMT in standard or urine samples. As no interference from common additives, excipients or drugs that can be commonly administered with BFMT is noticed, a previous extraction of the drug or the use of an internal standard is unnecessary. This makes the procedure simpler than other methods reported for this drug that use aqueous-organic mobile phases, where a previous extraction and an internal standard are recommended. Although dilution of urine samples is suggested in the proposed procedure, direct injection of the samples into the analytical column without any dilution is possible. Direct injection simplifies the handling and treatment of the sample.
In the literature, mobile phases containing significant amounts of the organic solvents methanol (~40% v/v) and acetonitrile (~35% v/v) are often used to achieve retention times for BFMT of ~11 and ~9 min, respectively. The micellar mobile phase used in the proposed procedure does not contain any organic solvent and gives good retention time for either analysis. The absence of organic solvents in the micellar mobile phase reduces the risk of changes in the mobile phase composition (because of the absence of volatile compounds), and the risk of flammability and contamination, which is of great interest for the control of toxic waste in laboratories and the health of chromatographers.
Acknowledgments
This study was part of Project BQU2001-3770, funded by MCYT-FEDER and the Project P1-1B2003-07, funded by Fundació Caixa de Castelló-Bancaixa. The authors would like to thank SCIC of the University Jaume I, Castellón, Spain, for the MS measurements.
References
(1) A.H. Hikal,
J. Liquid Chromatogr.
9
(13), 2937-2943 (1986).
(2) IOC, The Olympic Movement Anti-Doping Code, IOC, 2000 (http://
(3) R. Frontini and J.B. Mielck, J. Liquid Chromatogr. 15(14), 2519-2528 (1992).
(4) R. Frontini and J.B. Mielck, Eur. J. Pharm. Biopharm. 44, 85-88 (1997).
(5) M.E. Mohamed and H.Y. Aboul-Enein, Anal. Lett. 18, 2591-2603 (1985).
(6) C. Van Kerchove, R. Bontemps, and A. Shoenmakers, J. Pharm. Pharmacol.34, 420-424 (1982).
(7) M.I. Maguregui, R.M. Jimenez, and R.M. Alonso, J. Chromatogr. Sci. 36, 516-522 (1998).
(8) N.W. Smith and M.B. Evans, Chromatographia 41, 197-203 (1995).
(9) M. Schafer-Korting and E. Mutschler, Eur. J. Clin. Pharmacol. 21, 315-323 (1982).
(10) S.P. Agarwal and J. Nwaiwu, J. Chromatogr. 351, 383-387 (1986).
(11) S. Carda-Broch, J.S. Esteve-Romero, and M.C. GarcÃa-Alvarez-Coque, Analyst 123, 301-306 (1998).
(12) R.M. Smith, G.A. Murilla and T.G. Hurdley, J. Chromatogr. 384, 259-278 (1987).
(13) B. Beerman, M. Groschinsky-Grind, and B. Lindström, Eur. J. Clin. Pharmacol. 10, 293 (1976).
(14) C. Fagerlund, P. Hartvig, and B. Lindström, J. Chromatogr. 168, 107-116 (1979).
(15) J.A. Mollica, C.R. Rehm, and J. B. Smith, J. Pharm. Sci. 58, 635-636 (1969).
(16) J.A. Mollica et al., J. Pharm. Sci. 60, 1380-1384 (1971).
(17) A.R. Barnes and S. Nash, J. Clin. Pharm. Ther. 19, 89-93 (1994).
(18) A.R. Barnes and S. Nash, Int. J. Pharm. Ther. 94, 231-234 (1993).
(19) S. Carda-Broch, J. Esteve-Romero, and M.C. GarcÃa-Ãlvarez-Coque, J. Pharm. Biomed. Anal. 23, 803-817 (2000).
(20) S. Carda-Broch et al., Analyst 127, 29-34 (2002).
(21) M.C. GarcÃa-Ãlvarez-Coque and S. Carda-Broch, J. Chromatogr., B 736, 1-18 (1999).
(22) M.J. Ruiz-Angel et al., J. Chromatogr., A 947, 31-45 (2002).
(23) S. Carda-Broch et al., J. Chromatogr., A 893, 321-337 (2000).
(24) V. Ulvi and H. Keski-Hynnilä, J. Pharm. Biomed. Anal. 12, 917-922 (1994).
(25) V. Ulvi, J. Pharm. Biomed. Anal. 17, 77-82 (1998).
(26) E. Selvaag and P. Thune, Photodermatol. Photoimmunol. Photomed. 12, 79-83 (1996).
(27) D. Thieme et al., J. Chromatogr., B 757, 49-57 (2001).
(28) J.J. Alastair and M.D. Wood, N. Engl. J. Med. 339, 387-395 (1998).
Servei Central d'Instrumentació CientÃfica (SCIC), Universitat Jaume I, Castellón, Spain
*Area de QuÃmica AnalÃtica, Universitat Jaume I, Castellón, Spain, Address correspondence to S. Carda Broch.
MarÃa José Ruiz Angel previously worked as a technician at SCIC, Universitat Jaume I, (UJI) and currently has a postdoctoral fellowship from the Spanish Ministry of Education at the Laboratoire des Sciences Analytiques de l'Université Claude-Bernard, Lyon, France. Her research interests are on the use of ionic liquids in chemical analysis.
Mayte Gil Agustà is an assistant professor of analytical chemistry at Universitat Jaume I (UJI), Castellón, Spain, and performs research on drugs of abuse in biological fluids and formulations using micellar liquid chromatography (MLC).
Josep Esteve Romero is a professor of analytical chemistry and head of the Bioanalytical Research Group at Universitat Jaume I (UJI). He performs research on chemometrics applied to the analysis of biological samples using the LC and EC techniques.
Samuel Carda Broch is an assistant professor of analytical chemistry at Universitat Jaume I (UJI), working on photostability studies of products of biological interest in several matrices and conditions using LC.
Articles in this issue
almost 21 years ago
February TOCalmost 21 years ago
Peaks of Interestalmost 21 years ago
Short Coursesalmost 21 years ago
Fifty Years of GC Instrumentationalmost 21 years ago
Calendaralmost 21 years ago
HPLC Analysis of Nonvolatile Analytes Using Charged Aerosol Detectionalmost 21 years ago
Choice of Buffer for the Analysis of Basic Peptides in Reversed-Phase HPLCalmost 21 years ago
Extracolumn EffectsNewsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.