- Special Issues-10-01-2020
- Volume 18
- Issue 4
The Next Step in Targeted Drug Imaging for Oncology: Combining Laser-Induced Post-Ionization with MALDI Imaging
Over the last decade, matrix-assisted laser desorption–ionization (MALDI) imaging has become an indispensable tool for a broad range of applications, from studying plant metabolomics to discovering biomarkers of disease to developing new therapies. As such, MALDI imaging is revolutionizing preclinical drug discovery pipelines by providing direct distribution monitoring of therapeutic compounds and their metabolites along with untargeted pharmacodynamic information. A key application of MALDI imaging is tissue analysis for oncology, and recent developments in MALDI technology promise greater benefits to cancer research. The combination of MALDI with laser-induced post-ionization (PI) enhances the detection and imaging of pharmaceutical compounds and other classes of compounds, allowing for significant advances in the use of MALDI imaging for studying drug metabolism and pharmacodynamics in tumor tissues. This article describes the value of MALDI Imaging for oncology applications and examines the potential for laser-induced PI, including the ability to achieve up to three orders of magnitude higher sensitivity and to image metabolite classes previously undetectable with traditional MALDI.
Matrix-assisted laser desorption–ionization (MALDI) was initially designed as a mass spectrometry (MS) ionization method in the late 1980s (1). It was later developed into an imaging technique in 1994 to map the distribution of molecules from a thin sample, ranging from small metabolites to large proteins without molecular tags or labels (2). This approach was then extended to the analysis of tissue sections by Richard Caprioli and colleagues (3), whose groundbreaking studies demonstrated how MALDI-MS could be applied to visualize large biomolecules (such as proteins and lipids) in cells and tissues to reveal the distribution of these molecules and how distribution is changed by diseases such as cancer.
Significant technological and methodological advances over the last two decades have improved the performance of MALDI imaging, providing continuing enhancements in throughput and spatial resolution. Such developments have fueled the acceptance of this technology across a range of applications, including biomedical research fields such as oncology, neurology, cardiology, and rheumatology. When tissue-based imaging studies were first conducted with MALDI-MS, the method was primarily applied to analyzing the spatial distribution of proteins and delivering information about the distribution of single proteins, protein isoforms, and post-translational modifications (PTMs) (4). By using MALDI imaging, researchers could map hundreds of proteins simultaneously, unlike traditional immunohistochemistry (IHC) experiments.
Since then, MALDI imaging capabilities have been extended beyond traditional proteomics, to measure small molecules, metabolites, lipids, glycans, nucleic acids, and more. Another key advantage of MALDI-MS over techniques such as IHC is the ability to image unknown compounds. By using this untargeted approach, researchers can measure the molecular signatures of previously uncharacterized disease pathways.
MALDI Imaging in Oncology
A vast number of papers has been published on the use of MALDI imaging for cancer research applications. The technology has long been used both to discover and monitor potential therapeutic compounds and their metabolites, and to analyze tissue proteins for their potential clinical value for early diagnosis, prognosis, and prediction in cancer. Traditionally in pharmaceutical research and development (R&D), the discovery and development of safe and efficacious drugs has been based on measuring the parent drug in plasma. However, most drug targets found in plasma are dilute and downstream of the engagement site, so determining the relevant tissue distribution of the parent drug and its metabolites provides a greater understanding of pharmacology and toxicology profiles.
Conventional approaches, such as whole-body autoradiography (WBA) and liquid chromatography–mass spectrometry (LC–MS), provide some tissue-relevant information but are limited by the requirement for radioactively labeled probes and homogenized tissue extracts, respectively. MALDI imaging offers advantages over both approaches: As a label-free technique, MALDI imaging can detect parent drugs, metabolites, impurities, and degradation products as separate entities, generating important new information about the localization of drug compounds and important metabolites; and unlike LC–MS, MALDI imaging can provide spatial information about highly localized analytes, which could otherwise be overlooked by the extraction and homogenization process.
Biomarker Discovery
MALDI imaging is making significant contributions to the development of new biomarkers of disease, particularly in the field of cancer research. The heterogeneous nature of cancer cells and tissues makes preserving spatial integrity vital—a task well-suited to MALDI imaging. In particular, MALDI imaging has successfully detected previously unknown proteins in cancer and led to recent advances in the discovery of glycan biomarkers. In such studies, MALDI imaging has been used to characterize N-linked glycans in cancer tissues and develop tumor-specific glycan biomarkers.
It is estimated that over 50% of human proteins are glycosylated, making glycosylation one of the most common and complex PTMs (5). At the pathological level, changes in glycosylation are known to hold significance for tumor progression, but until recently it has not been effectively demonstrated. Using MALDI imaging for N-linked glycans, these processes can be directly localized in the tissue, to assign different glycans with different tissue features. For example, in a study of clear-cell renal cell carcinoma (ccRCC)—a prevalent subtype of kidney cancer typically detected at advanced stages with high resistance to chemotherapy and radiotherapy—MALDI imaging was able to identify multiple N-glycans that were increased in ccRCC (6). Figure 1 shows the N-glycan profiling of a representative ccRCC tissue selected because it had both tumor (Fuhrmann grade 2) and non-tumor sections separated by a fibrillar capsule. Continued evaluation of N-linked glycosylation and other glycan classes with MALDI imaging could help provide new therapeutic and diagnostic assay leads.
Diagnostic Potential
Cancer cells and other diseased tissues have significant genetic and epigenetic modifications that influence the genomic expression cascade. Whether studying the proteome, lipidome, or metabolome, the spatial distribution of compounds contains valuable information. Omics-based biomarker discovery can be limited without the benefit of spatial information to add important contextual clues because tissue-level communication networks are integral to cancer growth. MALDI imaging enables the identification of compounds that can act as predictive or prognostic biomarkers, and acts as a tool to stratify patients into appropriate treatment groups and predict responses to treatment (7).
Characterizing Tumor Subpopulations
Monitoring the progression of tumors is vital for the management and successful treatment of cancer. However, tumor heterogeneity represents a significant challenge to the development of effective drugs and accurate prognosis and diagnosis. MALDI imaging is becoming an increasingly relied upon tool to characterize this heterogeneity, by determining distinct tumor subpopulations and understanding localized molecular changes in detail.
One study combined MALDI imaging of lipids with deep proteomic coverage using LC–MS/MS for biomarker discovery and molecular characterization of breast cancer tumor subpopulations (8,9). Lipid imaging from tumor sections was used to define regions of interest (ROIs) by segmenting intratumor heterogeneity for laser microdissection (LMD)-based microproteomics (timsTOF fleX, Bruker Daltonics). Here, the ability to use the same tissue section for imaging, staining and LMD-based microproteomics is beneficial. After image processing, boundaries of the tumor sub-population areas were transferred to a coregistered optical image of a consecutive section and referenced to teach marks that were scanned together with the section (Figure 2). This allows coregistration of the MALDI imaging segment boundaries to the LMD for precise excision of the defined areas.
Protein extraction and tryptic digestion of small microdissected material was followed by proteomic analysis using parallel accumulation–serial fragmentation (PASEF). Analysis of proteomics data provided a comprehensive mechanistic understanding of cell-type specific biological processes in situ to complement the workflow.
Developments in Imaging Technology
The combination of MALDI-MS with ion mobility separation (IMS) has greatly broadened the range of compounds analyzed by MALDI imaging. IMS adds another dimension to mass spectrometric analysis. Over the last two decades, IMS has enabled fast separation and analysis of biomolecules in complex mixtures (such as tissue and cells), as isobaric lipid, peptide, and oligonucleotide molecular ions are preseparated in the mobility cell before mass analysis. There are numerous IMS technologies, but one that has recently contributed significant advances in tissue imaging is trapped ion mobility spectrometry (TIMS). The ability to separate ions by mobility using TIMS boosts sensitivity and provides additional selectivity by separating the ions by their collisional cross section (CCS).
The introduction of a MALDI TIMS imaging platform greatly enhances the chemical information that can be acquired from a single tissue section, improving the ability to fully investigate the molecular drivers of biological processes, such as cancer. However, the true quantum leap in sensitivity since MALDI was invented has arisen from the addition of laser-induced post-ionization (PI) (10), a technology developers at the University of Muenster. Studies have shown that this novel approach in- creases imaging sensitivity for many compounds by up to three orders of magnitude, expanding its utility particularly in drug metabolism and pharmacokinetics (DMPK) studies.
By enhancing molecular signals, laser-induced PI has allowed chemical classes that previously did not ionize with traditional MALDI to be imaged for the first time, particularly lipids, small molecules, and many drug compounds. For example, one study showed an increased signal in- tensity by up to two orders of magnitude for seven out of ten drug compounds analyzed by laser-induced PI compared with traditional MALDI analysis (11). This gain in sensitivity enabled the distributions of the drug compounds to be visualized, illustrating the potential of laser-induced PI imaging in pharmaceutical R&D.
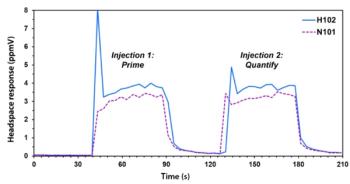
Steroids
Steroids are a biologically important class of compounds found ubiquitously in plants, animals, and fungi. There is significant interest in studying steroid distributions in tissues, but until now, such compounds did not ionize well using MALDI because of their nonpolar core structure. Many classes of steroids are commonly used in treating cancer, either directly to shrink tumors as part of chemotherapy, or as an anti-inflammatory agent or to treat nausea. Figure 3 shows the marked improvement in sensitivity with laser-induced PI compared with conventional MALDI imaging for three key steroids used in cancer treatment (12). Prednisolone showed a 100-fold increase in sensitivity, doxorubicin a 25-fold increase, and paclitaxel a >500-fold increase.
By imaging these compounds for the first time, researchers can better understand the distribution of steroids in tissues and improve how they are used in cancer treatments.
Ongoing Innovation
The introduction of laser-induced PI to imaging is set to revolutionize clinical research and, in time, has the potential to benefit clinical diagnostics, particularly in the field of oncology. Laser-induced PI has now been applied to a dual MALDI–electrospray ionization (ESI) mass spectrometer, combining high mass accuracy with advanced MALDI imaging for the separation and identification of analytes in complex mixtures, such as lipids and glycans (13). As this novel technique develops in the coming years in line with state-of-the-art mass spectrometers, doors will continue to open for transforming the discovery of novel cancer biomarkers, and improve treatment options, prognoses, and diagnoses.
References
(1) M. Karas, D. Bachmann, and F. Hillenkamp, Anal. Chem. 57(14), 2935–2939 (1985).
(2) B. Spengler, M. Hubert, and R. Kaufmann, “MALDI ion imaging and biological ion imaging with a new scanning UV-laser microprobe,” paper presented at the 42nd American Society for Mass Spectrometry Conference, Chicago, IL, USA, 1994.
(3) R.M. Caprioli, T.B. Farmer, and J. Gile, Anal. Chem. 69(23), 4751– 4760 (1997).
(4) M. Stoeckli, P. Chaurand, D.E. Hallahan, and R.M. Caprioli, Nat. Med. 7, 493–496 (2001).
(5) R.R. Drake, T.W. Powers, E.E. Jones, E. Bruner, A. Mehta, and P.M. Angel, Adv. Cancer Res. 134, 85–116 (2017).
(6) R.R. Drake, C. McDowell, C. West, F. David, T.W. Powers, T. Nowling, E. Bruner, A.S. Mehta, P.M. Angel, L.A. Marlow, H.W. Tun, and J.A. Copland, J. Mass. Spectrom. 55, 44–90 (2020).
(7) A. Ly, M. Aichler, and A. Walch, Hospital Healthcare Europe. https:// hospitalhealthcare.com (accessed 2013).
(8) J. Oetjen, R. Hebeler, F. Dewez, C. Henkel, B. Balluff, and R. Heeren, “MALDI guided SpatialOMx uncovers proteomic profiles in tumor subpopulations of breast cancer,” Application Note, Bruker Daltonics (2020).
(9) F. Dewez, J. Oetjen, C. Henkel, R. Hebeler, H. Neuweger, E. De Pauw, R.M.A. Heeren, B. Balluff, Proteomics (2020) https://doi.org/10.1002/ pmic.201900369.
(10) J. Soltwisch, H. Kettling, S. Vens-Cappell, M. Wiegelmann, J. Müthing, and K. Dreisewerd, Science 348, 211–215 (2015).
(11) F.P.Y Barré, M.R.L. Paine, B. Flinders, A.J. Trevitt, P.D. Kelly, R. Ait-Belka- cem, J.P. Garcia, L.B. Creemers, J. Stauber, R.J. Vreeken, B. Cillero-Pas- tor, S.R. Ellis, and R.M.A. Heeren, Anal. Chem. 91(16), 10840–10848 (2019).
(12) “Caution! MALDI-2 detects analyte classes never seen before,” Application Note, Bruker Daltonics (2020).
(13) J. Soltwisch, B. Heijs, A. Koch, S. Vens-Cappell, J. Höhndorf, and K. Dreisewerd, Anal. Chem. 92(13), 8697–8703 (2020).
Shannon Cornett, PhD, is an Applications Development Manager with Bruker Daltonics in Billerica, Massachusetts. Direct correspondence to: shannon.cornett@bruker.com
Articles in this issue
Newsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.