- LCGC North America-06-01-2017
- Volume 35
- Issue 6
Applicability of Hydrogen–Deuterium Exchange in Comparing Conformations of Innovator to Biosimilar Biopharmaceutical Products

Significant recent advances now enable routine usage of HDX-MS for comparing the conformations of biopharmaceutical products.
As the biopharmaceutical industry has grown, more and more drugs are coming off patent, leading to an increase on worldwide markets of biosimilars that compete with the innovator drugs. All regulatory agencies are carefully monitoring just how closely a biosimilar company can mimic the innovator product, with similar or identical safety, efficacy, and therapeutic properties. Here we discuss the potential applications of hydrogen–deuterium exchange mass spectrometry (HDX-MS) to determine similarities in the higher-order structures of a biosimilar and its innovator drug.
As the biopharmaceutical industry has grown, more and more innovator (also known as proprietary) drugs are coming off patent, and more biosimilars are appearing on the worldwide markets competing with the innovator drugs for sales, adoption, marketing, and acceptance. This nuance in the existing biopharmaceutical markets can and will include peptides, proteins, antibodies (monoclonal antibodies [mAbs]), fusion proteins, antibody–drug conjugates (ADCs), and virtually any other biopharmaceutical product ever known. The attraction for introducing biosimilars, which more biopharma companies are doing today, lies in being able to mimic the proprietary product in every imaginable way, so that chemically and biologically they are identical to the proprietary versions (1). If chemical equivalency and reproducible bioprocesses can be satisfactorily demonstrated to the regulatory agencies, then the need for extensive animal or human clinical trials may be abrogated. In theory, as we see it now, that could save the biosimilar companies an enormous amount of time, manpower, resources, and money in bringing biosimilars to market. Thus, all regulatory agencies are carefully monitoring just how closely a biosimilar company is able to mimic the innovator product, with similar or identical safety, efficacy, and therapeutic properties. However, unlike the generics of small-molecule drugs, exact replicas are much more difficult to be made of biologics because of their structural complexity and complicated manufacturing processes (2,3). This is especially true for high-molecular-weight proteins, specifically mAbs, fusion proteins, and ADCs. It is the inherent and intrinsic complexity and heterogeneity of mAbs and related products, as well as the changes that can come about by small differences in the manufacturing process, expression system makeup, and small changes often present in the glycosylation patterns, that can lead to potential complications associated with the introduction of biosimilars to the marketplace around the world.
Demonstrating the unequivocal chemical and biological equivalencies, without doing animal or human clinical trials to establish safety and efficacy, can become a tricky, slippery slope for the new biosimilar and regulatory agencies. Nevertheless, numerous biosimilars have been successfully brought to market in Europe, Japan, India, and recently, the United States, with more to surely follow (1,2). We have recently discussed the possible validation requirements for biopharmaceuticals (4), as well as possible analytical methods that can be used when comparing the innovator with its biosimilar, so far as specific attributes or chemical characteristics are concerned (5). There are numerous approaches already described for successful comparisons of various physical or biological properties between these two classes (5–7). What appears lacking from the existing analytical literature is a direct method for allowing unequivocal, structural, equivalency demonstrations between a biosimilar and its proprietary originator, especially having to do with higher-order structures (HOS) and their comparisons (8–10). We are aware that the United States Food and Drug Administration (FDA) is now receiving submittals for biosimilars and innovator biopharmaceutical drugs using, amongst other methods, hydrogen–deuterium exchange mass spectrometry (HDX-MS) to compare HOS (11). As far as we know, it is not yet clear if such FDA submittals contain direct comparisons between a biosimilar and its innovator analog, but there is every reason to expect this will transpire.
Problems with Existing Analytical Methods for Comparisons of Biosimilars and Innovators
Why are we specifically going to discuss the potential applications of HDX-MS to determine similarities in the HOSs between a biosimilar and its innovator drug? Are there not enough analytical methods already known that can perform such direct structural comparisons? In reality, there are only a few analytical methods that can detail HOS for biopharmaceuticals under biological conditions, which is really what is needed. Though nuclear magnetic resonance (NMR) spectroscopy and X-ray methods can indeed detail HOS, they require very special conditions and solvents (NMR) or solid-state conditions (NMR and X-ray), that are far from the usual, biological conditions where biopharmaceuticals act. Thus, even if such methods could detail HOS for both proprietary and biosimilar products, those conditions do not mimic biologically necessary buffers or approach conditions in the body. Many of these analytical methods, despite the requirement for very expensive instrumentation with extensive computerization and serious expertise to operate, still do not produce results that relate to the medium used to determine biological activity, safety, and efficacy in vivo.
Methods such as Fourier transform-infrared (FT-IR) spectroscopy, Raman spectroscopy, circular dichroism (CD) spectroscopy, differential scanning calorimetry (DSC), or isothermal calorimetry (ITC) can be applied, but they do not really provide the needed spatial resolution. While CD can indeed predict the percent random coil, beta sheet, or alpha helix present in a protein, it does not specify where each of these elements exist. CD does not show actual, absolute conformational analysis, nor does FT-IR, Raman, or any other spectroscopic method. These methods provide a global sum of all structural elements. In some cases, to be functional, the proteins of interest can contain some buffers that are not amenable to CD, FT-IR, or Raman spectroscopy.
HDX-MS Capabilities
It has been suggested that when comparing biosimilars and innovators, differences exist between these two classes of biopharmas, usually because the methods of expression are almost always different. Even small differences in their glycosylation patterns, which are often the case, can disturb conformations to the point where, at least in those regions, true differences in HOS do exist, and the final product may lose its efficacy leading to unwanted side effects. However, it may be difficult to determine the in vivo conformational changes between these protein types. As of now, neither HDX-MS nor other high-resolution structural methods are able to define the true in vivo conformation of proteins. However, unlike some methods, HDX-MS can investigate proteins under many conditions, including those that are as near to physiological as possible (that is, buffer components, pH, and so forth) where the proteins that are interrogated are functionally active in biological assays.
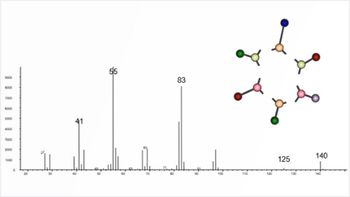
In general, for the majority of applications in the biopharmaceutical industry, HDX-MS depends on enzymatically cleaving the protein of interest (usually with pepsin) into peptic peptides. As a first step, digestion is done for the starting material, before any deuterium exchange, and then, of course, after establishing all the conditions necessary for obtaining a good protein coverage, deuterium exchange is initiated as a function of time. Changes in the degree of deuteration versus time are indicative of alterations in backbone amide environments, some regions may undergo more deuterium exchange than others only because their amide hydrogens are less protected from exchange. Changes in conformations will be demonstrated by different amounts of deuteration, because the protein has become more unfolded, or dynamic, or it has assumed a different conformation, as a function of temperature, solvents, pH, stress, and so forth. However, unlike NMR or X-ray crystallography this method cannot define protein structure because it cannot differentiate secondary structure. Under a multitude of experimental conditions (mutations, pH, temperature, buffers, additives, and so forth), this technique can distinguish very well between two or more conformations, where certain sections will undergo more or less deuteration, as a function of such conditions or not. These differences in deuterium uptake are then indicative of changing protein conformations for a single given protein or, when comparing two different states of the very same protein, differences in the amount of deuterium uptake by one conformation will become obvious. Unless the conformation is known from a previous high-resolution structure, HDX-MS still does not reveal the actual conformation of the proteins that were interrogated. Similarly, changes in the solution conditions or temperature of a protein can induce changes in the biological conformation. These changes will show up as differences in the deuterium uptake for certain sections of that protein, vis-à-vis individual peptide fragments after digestion. These are all useful phenomena, as illustrated below, when we discuss first how HDX-MS has been used to define changes in HOSs of individual biotherapeutic proteins. Later, we address how HDX-MS has been used to compare a proprietary versus biosimilar protein, all from the existing literature.
Introduction to HDX-MS and How It Is Used to Define HOS
More than 25 years ago, HDX coupled with MS was used for the first time to study protein conformation and dynamics (12). Since that milestone, HDX-MS has undergone tremendous changes, making it a turnkey solution to study protein conformations in numerous environments (13). HDX-MS has been widely used in the biopharmaceutical industry for HOS characterization of protein therapeutics, in research and development (R&D) (Figure 1). In part, this has been because of an automated platform and commercial availability of data analysis software (14–17).
A strong attribute of the HDX-MS method is its ability to study protein conformation and dynamics in a “native-like” environment. That, combined with the sensitivity and resolution of MS, offers considerable analytical power to interrogate all sorts of proteins from small (18) to megadalton complexes (19). Among the advantages of implementing this method compared to X-ray crystallography and NMR are small sample consumption (low micromolar range), no protein size limitation, tolerability of multiple buffer compositions (for example, detergents, nanodiscs, and liposomes) and most recently, in some cases, amino acid resolution (20–22).
When a protein is exposed to D2O, the backbone NHs, as well as some side chain H atoms, can be exchanged with D. In HDX-MS implementations, one can monitor only the exchange into the backbone amide H’s, as the other exchangeable H’s are quite labile and will rapidly back-exchange during liquid chromatography (LC)–MS analysis (23). By monitoring the protein backbone amide H’s, which depend on the protein local solvent accessibility and H bonds, solution conformation and dynamics of proteins can be interrogated, including changes because of the external environment (24)-such as chemical modifications (25,26), buffer composition (27), and protein-protein (ligand) interactions (28). The resulting data give information about protein conformation, in solution, and it can obtain structural information about a multitude of conditions: protein folding, effects of mutation on a protein, effects of post-translational modifications (PTMs) on protein structure, protein–protein interactions, protein–small molecule interactions, and so on. Effects on the protein conformation by formulation buffers, protein concentration, and excipients can also be investigated with HDX-MS, making the method suitable for the biopharmaceutical industry (Figure 1).
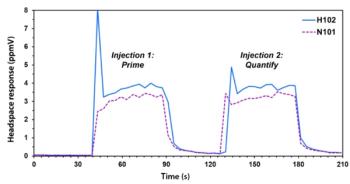
In continuous labeling HDX-MS experiments (Figure 2), protein samples are labeled with excess D2O, and at different time points, the exchange reaction is quenched by lowering the pH to 2.5 and the temperature to 0 °C. This step is crucial to retain D on the labeled protein because the exchange reaction is dependent on temperature and pH (29–31). The deuterated samples are frozen or injected immediately in a precooled LC system to limit back-exchange (32). Labeled samples can either be analyzed at the global level, where the exchange data reports on the overall exchange of the entire molecule, or at the peptide level, by doing on-line or off-line pepsin digestion, where the results provide better spatial resolution. Other acid proteases can also be used for digestion (33–37). After protease digestion, peptides are separated and detected by LC–MS. Multiple software packages are available that can help with data analysis and interpretation (16). Although this review is not intended to cover all published HDX-MS papers on HOS, we focus first on a few papers that had an impact for the study of biotherapeutics.
HOS Characterization of Antibodies
Among proteins, mAbs are the largest and fastest growing therapeutics, with >40 mAbs approved by the FDA, along with >300 mAb candidates in development (38). To understand the conformation of a recombinant, monoclonal IgG1 antibody, pioneering HDX-MS work by Houde and colleagues was performed at global and local levels (39). These studies showed that IgG1 exists in a well-deï¬ned conformation, with regions highly protected from H exchange, and other dynamic and ï¬exible regions. By using HDX-MS, the effects of methionine oxidation, fucosylation, and galactosylation on an intact IgG1 were evaluated, and their effects on IgG1 binding to the Fcg RIIIa receptor (25). This work showed that different glycan structures mediate binding with FcgRIIIa, by increasing the rigidity of the CH2 domain. Others applied HDX-MS to three major disulï¬de isoforms of IgG2, namely, IgG2-B, IgG2-A1, and IgG2-A2 (40). This provided some rationale for the stability and antigen binding potency of different mAbs, as more ï¬exible regions would be more accessible for antigen binding. Iacob and colleagues studied protein aggregation of a mAb by HDX-MS, and the data indicated regions prone to aggregation (41). In a recent publication (42), the authors present an approach to obtain high-resolution HDX-MS data in mAbs. They are investigating the rate of asparagine deamidation in mAbs using HDX-MS. In this paper (42), the authors compared two antibodies with different specificities that share a canonical NG motif that is prone to deamidation in one of the antibodies but not in the other.
ADCs have also been successfully interrogated with HDX-MS to monitor effects of a payload conjugated toxin on a mAb. Pan and colleagues used HDX-MS to study monomethyl auristatin E or F, conjugated with a monoclonal antibody (43). The results showed that the ADCs and mAbs share similar conformations and dynamics in solution, demonstrating that the drug conjugation does not induce conformational changes on the protein. Such studies demonstrated the usefulness of HDX-MS to expand our understanding of HOS in ADCs, and other biotherapeutics (44,45).
HOS Characterization of Other Biotherapeutics and Interactions
Other therapeutic proteins (46,47), such as fusion proteins, interferon, and enzymes, have also been studied by HDX-MS. Recent papers used a specific protein drug, interferon beta-1a (IFN), to illustrate the possible utility of HDX-MS as a powerful tool not only to assess the integrity of HOS, but also to predict the consequences of its degradation under various conditions (48,49). All of the MS methods used, not just HDX-MS, demonstrated small changes in the HOS of IFN as it underwent various preparations, treatments, and chemical modifications, such as native versus denatured, native versus chemically alkylated IFN, and others. Huang and colleagues (50) investigated the role of the aggregation propensity of an Fc-fusion protein therapeutic, and the data revealed a potential aggregation interface in the Fc domain. This provided a general strategy for characterization of aggregation propensity of Fc fusion proteins at a molecular level.
One of the more sought after utilities of HDX-MS has been to investigate protein–protein or protein–ligand interactions (13). Malito and colleagues probed the binding between a monoclonal antibody and factor H binding protein (fHbp), the vaccine antigen of Neisseira meningitides (51). The epitope was probed with peptide arrays, phage display, X-ray crystallography, and HDX-MS. Others implemented HDX-MS for the interactions between the extracellular domains of EGFR with a small biotherapeutic, a monobody-adnectin. HDX-MS data revealed insights into the dynamics of EGFR and was in very good agreement with the X-ray crystal structure (52).
HDX-MS Used to Compare Innovators with Biosimilars
The intent in this section is to discuss specific examples when HDX-MS was used to make comparisons between innovator drugs and their biosimilar versions. On this topic, there are not too many publications that address the comparability between innovators and biosimilars using HDX-MS, but we found several articles discussing this subject. Perhaps one of the best reviews is by Beck and colleagues, which shows how HDX-MS is implemented to compare originator (innovator) to biosimilar and biobetter antibodies (53). Another article that we found by Visser and colleagues (54) discusses a single, direct comparison between innovator and biosimilar, rituximab, a therapeutic mAb for treatment of non-Hodgkin’s lymphoma and chronic, lymphocytic leukemia (54).
To better understand the physicochemical and functional comparability between the innovator and biosimilar, an array of orthogonal analytical methods and biological characterizations were performed (53,54). In the paper by Visser and colleagues, HDX-MS showed that GP2013 and rituximab originator showed the same conformations, even when using different cell lines and manufacturing (54). The biosimilar was highly similar to the innovator, at the level of primary and HOS, PTMs, and biological properties. This was one of the earlier demonstrations that biosimilars could be developed for mAbs, which has continued and will continue indefinitely. The manuscript nicely summarized the analytical toolbox used for the physicochemical, HOS, and functional characterization of biosimilar and original rituximab (54). Protein labeling methods, such as HDX-MS, are often used to indicate small differences in HOS at the peptide level. In the same paper by Visser and colleagues (54), similar deuterium exchange rates were seen for GP2013 and the innovator product. HDX-MS can be seen to be much more specific about where conformational differences could exist, when comparing two such products. For an individual protein, it does not provide absolute, structural conformations but only what sections of the protein are able to undergo H–D exchange.
Another recent publication by Fang and colleagues described the comparison of remicade (reference) and inflectra (biosimilar) via multivalent approaches (8). They described comparisons of glycan profiles showing a high degree of similarity, with small differences for lower abundance glycans. In comparing HOS, they used HDX-MS to further confirm the similarity of the pair. There were very small differences that were not meaningful (49) in the apparent conformations, close to the location of the glycan site. These changes suggested that slight differences in glycan composition at the glycosylation site (N297) lead to small conformational changes between the innovator and biosimilar that don’t affect the function of the biosimilar. Glycan changes often come about because of slight differences in expression and manufacturing processes or manufacturing firms. To interpret and visualize conformational changes between proteins that are compared, HDX-MS data can be displayed in different ways as described below.
Ways to Look at HDX-MS Data
In making good and clear comparisons, as just described, data display can be critical. HDX-MS data can be summarized using a variety of formats.
For individual, single proteins, the deuterium incorporation is determined by extracting the data from the mass spectrometer, and plotting data in a D incorporation graph that shows the amount of D incorporated as a function of time for each peptide (Figure 2). A heat map can be generated (not shown here), showing the relative amount of D incorporation versus time for each identified peptide. Comparison heat maps can then compare two different proteins states, or an innovator versus a biosimilar. In the study by Fang and colleagues (8), the data were compared using a butterfly plot (Figure 3a) as described in the publication of Houde and colleagues (49). By plotting the data in that way, it aided in rapidly enabling both the qualitative and quantitative assessment of comparability. The butterfly plot contains the average, relative fractional exchange data for innovator (top) versus biosimilar (bottom), as a function of peptide location. Conformational differences, would appear as differences in the differential plot, away from zero (not the case in Figure 3). The standard deviation (SD) between any two measurements across all peptides was <±0.05 Da, within the experimental error. Again, this must mean, in terms of tertiary structures, that the biosimilar sample is very comparable to the reference. Measured small differences in heavy and light chains are within experimental error, hence not real. Thus, there are no meaningful changes in the degree of D incorporation between these two proteins. The HDX-MS data presented by Fang and colleagues (8) strongly pointed to identical conformations between these two mAbs. These same type of studies can also be used to compare complementarity determining regions (CDR) of mAbs, and to conclude if they are the same in their abilities to recognize the antigenic species. From all these publications, the authors conclude that HDX-MS is capable of providing more informative and confident comparability assessments for protein HOS than what is currently available via other methods, with time and costs being equal.
Bottom-Up and Top-Down Approaches for HDX-MS
HDX-MS approaches have become very commonplace and have been duplicated for other pairs of proprietary and biosimilar drugs. For example, Pan and colleagues recently described a comparison of HOS analysis of mAbs using bottom-up and top-down HDX-MS methods (55). Here they analyzed two bevacizumab (BEV) biosimilars to the reference BEV using two different sequencing methods. Prior work only used a single method, either peptide-based bottom-up sequencing HDX or a protein-based, top-down sequencing HDX approach, but never both together. We have reviewed top-down sequencing (56). Different extents of coverage of the antibody (BEV) sequence were obtained with the two methods, neither of which was 100% for both heavy and light chains, combined. The D incorporation behavior for the peptides from the three samples of BEVs were compared, side-by-side, and they showed zero differences at various HDX time points. The same ways of representing data, as explained above-for example, heat maps, mirror image plots, butterfly plots, and so forth-were used here (8). Neither top-down sequencing nor bottom-up sequencing provided 100% sequence coverage alone. However, the peptide information from the bottom-up sequencing, and the residue level and intact subunit information from the top-down sequencing, were complementary leading to 100% coverage for the mAb. Both the bottom-up and top-down sequencing approaches indicated the three BEV samples had no differences in HOSs (55). It was also concluded that top-down sequencing was better suited for detecting subtle differences. These might qualify or disqualify the performance of a new drug, as inferred from the HDX results. The top-down sequencing approach could provide significant benefits in other instances and applications where structural differences do exist. Electron-transfer dissociation (ETD) or electron-capture dissociation (ECD)-based top-down sequencing methods are also able to perform better than NMR when interrogating the HOS of very high MW proteins. As top-down sequencing improves and grows in usage, especially with commercial improvements (for example, ultraviolet photodissociation [UVPD]), the residue-level information and the intact subunit-level information should increase. Today, top-down sequencing alone does not achieve 100% sequence and HDX coverage for proteins.
One final recent report also dealt with direct comparisons of reference versus biosimilar proteins. The paper compared SB4 (benepali), as the biosimilar to its reference, enbrel (58). The quality assessment of SB4 was performed according to the The International Conference on Harmonization (ICH) comparability guidelines and the biosimilar guidelines of the European Medicines Agency (EMA) and FDA. In a second example, SB2 (flixabi and renflexis) was the biosimilar to remicade (infliximab). The development of SB2 and its comparison with its reference material, using HDX-MS in part, was performed in accordance with relevant guidelines from the ICH, EMA, and FDA (58). Such studies have now become commonplace in the literature and mimic our comparison of proprietary versus biosimilars.
Conclusions and Future Directions
In summary, biopharmaceutical comparability rests upon the idea that modern analytical chemistry and biology (bioassays) can suggest if comparability exists between samples of biopharmaceuticals. This ability depends on criteria that may not be 100% straightforward or obvious. The adoption of a certain three-dimensional (3D) structure, actually a composition of conformations at any given time, temperature, and solvents, is required for proteins to perform their intended function. If changes to HOS occur, it can compromise a biopharmaceutical’s function or cause adverse effects. Thus, it is obvious that consistent production of protein biopharmaceuticals, both innovators and biosimilars, must manufacture products that have the same, or very comparable, folded structures. This can come about via having improved analytical information. The US FDA has started to receive submittals containing HDX-MS data for both biosimilars and proprietary biopharmaceuticals. And, these submissions have come from companies applying for permission to enter partial clinical trials or marketing of the final drugs (11).
There have been very significant advances within the past several years (59) that permit routine usage of HDX-MS for comparisons of conformations between a proprietary and a biosimilar. Complete automation and easy software access is now a viable reality, at least from three major suppliers. The ability to apply such complex instrumentation, often with robotic control of sample handling at the front, is routine in many academic and biopharmaceutical laboratories. Quality control, quality assurance, and everything that has become routine with regulatory agency requirements for biopharma firms, can now be routinely applied to HDX-MS. It is not just comparing biosimilars to innovator drugs, but different batches for production and process control of both types of biopharmaceuticals is now practical and feasible.
The operational requirements in applying HDX-MS for the above types of applications has been fully demonstrated by several laboratories and biopharmaceutical companies (13). Future improvements would be to save time and manual efforts in routinely applying HDX-MS. This calls for more automation of instrumentation, sample handling, data handling, and interpretation by computer-controlled data stations. There is every reason to expect that HDX-MS will continue to expand and, perhaps, even dominate how we investigate HOSs for all biopharmaceuticals. Our ability to make valid and binding comparisons between biosimilars, biobetters, and proprietary biopharmaceuticals is now possible on a regular and routine basis. These are significant advances for bringing certain biopharmaceuticals to market successfully, faster, and safer than before.
References
- H. Mellstedt, Eur. J. Cancer, supplements, 11(3), 1–11 (2013).
- European Medicines Agency, “Guideline on Similar Biological Medicinal Products Containing Monoclonal Antibodies − Non-clinical and Clinical Issues” (EMA, London, United Kingdom, Committee for Medicinal Products for Human Use, 2012).
- M. Weise et al., Nat Biotechnol.29, 691−3 (2011).
- I. Apostol, I. Krull, and D. Kelner, in Analytical Chemistry, I.S. Krull, Ed. (InTech- Open Access Publishers, Rijeka, Croatia, November, 2012). Available at:
http://www.intechopen.com/articles/show/title/analytical-method-validation-for-biopharmaceuticals . - D. Wilkinson, A.S. Rathore, and I.S. Krull, LCGC North Am.35(1), 36–44 (2017).
- R.J. Falconer, D. Jackson-Matthews, and S.M. Mahler, J. Chem. Technol. Biotechnol.86, 915–922 (2011).
- M.A. Alsenady, N.K. Jain, J.H. Kim, C.R. Middaugh, and D.B. Volkin, Front. Pharmacol.5, 1–19 (2014).
- J. Fang, C. Doneanu, W.R. Alley, Jr., Y.Q. Yu, A. Beck, and W. Chen, mAbs8(6), 1021–1034 (2016).
- J. Pan, S. Zhang, and C.H. Borchers, Biochim. Biophys. Acta1864, 1801–1808 (2016).
- B. Deng, C. Lento, and D.J. Wilson, Anal. Chim. Acta940, 8–20 (2016).
- “Workshop on Biopharmaceutical Analysis Methods,” presented at the 2016 American Society Mass Spectrometry National Meeting (ASMS), San Antonio, Texas, 2016.
- V. Katta and B.T. Chair, RCMS5, 214–217 (1991).
- G.F. Pirrone, R.E. Iacob, and J.R. Engen, Anal. Chem.87, 99–118 (2015).
- R.Y.C. Huang and G.D. Chen, Anal. Bioanal. Chem.406, 6541–6558 (2014).
- H. Wei, J. Mo., L. Tao, R.J. Russell, A.A. Tymiak, G. Chen, R.E. Iacob, and J.R. Engen, Drug Discov. Today19, 95–102 (2014).
- J. Claesen and T. Burzykowski, Mass Spectrom. Revs.36(1), DOI: 10.1002/mas.21519 (2016).
- U. Leurs, U.H. Mistarz, and K.E. Rand, Official J. Arbeitsgemeinschaft, Pharmaz. Verfahr. E.V,93, 95–109 (2015).
- J.R. Engen, T.E. Wales, S. Chen, E.M. Marzluff, K.M. Hassell, D.D. Weis, and T.E. Smithgall, Intl. Revs. Phys. Chem. 32, 96–127 (2013).
- J.Z. Bereszczak, R.J. Rose, E. van Dujin, N.R. Watts, P.T. Wingfield, A.C. Steven, and A.J. Heck, J. Am. Chem. Soc.135, 6504–6512 (2013).
- K.D. Rand, C.M. Adams, R.A. Zubarev, and T.J. Jorgensen, J. Am. Chem. Soc.130, 1341–1349 (2008).
- K.D. Rand and T.J. Jorgensen, Anal. Chem.79, 8686–8693 (2007).
- K.D. Rand, M. Zehl, O.N. Jensen, and T.J. Jorgensen, Anal. Chem. 81, 5577–5584 (2009).
- J.R. Engen, Anal. Chem.81, 7870–7875 (2009).
- J.J. Skinner, W.K. Lim, S. Bedard, B.E. Black, and S.W. Englander, Protein Sci. 21, 996–1005 (2012).
- D. Houde, Y. Peng, S.A. Berkowitz, and J.R. Engen, Mol. Cell. Proteomics9, 1716–1728 (2010).
- H. Wei, J. Ahn, Y.Q. Yu, A. Tymiak, J.R. Engen, and G.D. Chen, J. Am. Soc. Mass Spectrom.23, 498–504 (2012).
- R. Majumdar, P. Manikwar, J.M. Hickey, H.S. Samra, H.A. Sathish, S.M. Bishop, C.R. Middaugh, D.B. Volkin, and D.D. Weis, Biochem. 52, 3376–3389 (2013).
- M.J. Chalmers, S.A. Busby, B.D. Pascal, G.M. West, and P.R. Griffin, Expert Rev. Proteomics8, 43–59 (2011).
- S.W. Englander, J. Am. Soc. Mass Spectrom.17, 1481–1489 (2006).
- Y. Bai, J.S. Milne, L. Mayne, and S.W. Englander, Proteins17, 75–86 (1993).
- G.P. Connelly, Y. Bai., M.F. Jeng, and S.W. Englander, Proteins17, 87–92 (1993).
- T.E. Wales and J.R. Engen, Mass Spectrom. Rev.25, 158–170 (2006).
- L. Crabvello, D. Lasoucx, and E. Forest, Rapid Commun. Mass Spectrom.17, 2387–2393 (2003).
- H.M. Zhang, S. Kazazic, T.M. Schaub, J.D. Tipton, M.R. Emmett, and A.G. Marshall, Anal. Chem. 80, 9034–9041 (2008).
- J. Marcoux, E. Thierry, C. Vives, L. Signor, F. Fieschi, and E. Forest, J. Am. Soc. Mass Spectrom.21, 76–79 (2010).
- M. Rey, P. Man, G. Brandolin, E. Forest, and L. Pelosi, Rapid Commun. Mass Spectrom.23, 3431–3438 (2009).
- J. Ahn, M.J. Cao, Y.Q. Yu, and J.R. Engen, Biochim. Biophys. Acta1834, 1222–1229 (2013).
- D.M. Ecker, S.D. Jones, and H.L. Levine, mAbs7, 9–14 (2015).
- D. Houde, J. Arndt, W. Domeier, S. Berkowitz, and J.R. Engen, Anal. Chem.81, 2644–2651 (2009).
- A. Zhang, J. Fang, R.Y. Chou, P.V. Bondarenko, and Z. Zhang, Biochem.54, 1956–1962 (2015).
- R.E. Iacob, G.M. Bou-Assaf, L. Makowski, J.R. Engen, S.A. Berkowitz, and D. Houde, J. Pharm. Sci.102, 4315–4329 (2013).
- J.J. Phillips, A. Buchanan, J. Andrews, M. Chodorge, S. Sridharan, L. Mitchell, N. Burmeister, A.D. Kippen, T.J. Vaughan, D.R. Higazi, and D. Lowe, Anal. Chem. DOI:10.1021/acs.analchem.6b04158 (2017)
- L.Y. Pan, O. Salas-Solano, and J.F. Valliere-Douglass, Anal. Chem.86, 2657–2664 (2014).
- J.F. Valliere-Douglass, S.M. Hengel, and L.Y. Pan, Mol. Pharm. 12, 1774–1783 (2015).
- R.Y. Huang and G. Chen, Drug Discov. Today21, 850–855 (2016).
- D. Houde and S.A. Berkowitz, J. Pharm. Sci.101, 1688–1700 (2012).
- C.E. Bobst, J.J. Thomas, P.A. Salinas, P. Savickas, and I.A. Kaltashov, Protein Soc. 19, 2366–2378 (2010).
- I.A. Kaltashov, C.E. Bobst, R.R. Abzalimov, S.A. Berkowitz, and D. Houde, J. Am. Soc. Mass Spectrom. 21, 323–337 (2010).
- D. Houde, S.A. Berkowitz, and J.R. Engen, J. Pharm. Sci.100(6), 2071–2086 (2011).
- R.Y. Huang, R.E. Iacob, S.R. Krystek, M. Jin, H. Wei, L. Tao, T.K. Das, A.A. Tymiak, J.R. Engen, and G. Chen, J. Am. Soc. Mass Spectrom. DOI: 10.1007/s13361-016-1452-7 (2016).
- E. Malito, A. Faleri, P. Lo Surdo, D. Veggi, G. Maruggi, E. Grassi, E. Cartocci, I. Bertoldi, A. Genovese, L. Santini, G. Romagnoli, E. Borgogni, S. Brier, C. Lo Passo, M. Domina, F. Castellino, F. Felici, S. van der Veen, S. Johnson, S.M. Lea, C.M. Tang, M. Pizza, S. Savino, N. Norais, R. Rppuoli, M.J. Bottomley, and V. Masignani, Proc. Natl. Acad. Sci. U.S.A.110, 3304–3309 (2013).
- R.E. Iacob, G. Chen, J. Ahn, S. Houel, H. Wei, L. Mo, L. Tao, D. Cohen, D. Xie, Z. Lin, P.E. Morin, M.L. Doyle, A.A. Tymiak, and J.R. Engen, J. Am. Soc. Mass Spectrom.25, 2093–2102 (2014).
- A. Beck, F. Debaene, H. Diemer, E. Wagner-Rousset, O. Colas, A. Van Dorsselaer, and S. Cianferani, J. Mass Spectrom.50, 285–297 (2015).
- J. Visser, I. Feuerstein, T. Stangler, T. Schmiederer, C. Fritsch, and M. Schiestl, BioDrugs27, 495–507 (2013).
- J. Pan, S. Zhang, and C.H. Borchers, Biochim. Biophys. Acta1864, 1801–1808 (2016).
- I.S. Krull, A. Rathore, and J.A. Loo, LCGC North Am. 34(7), 492–499 (2016).
- D. Houde and J.R. Engen, Chim. Oggi/ Chem. Today27(2), 12–15 (2009).
- J. Hong et al., mAbs 0.1–19, http://dx.doi.org/10.1080/19420862.2016.126455 (2017).
Hydrogen Exchange Mass Spectrometry of Proteins: Fundamentals, Methods, and Applications, D.D. Weis, Ed. (John Wiley & Sons, West Essex, UK, 2016).
John R. Engen is a Distinguished Professor in the Department of Chemistry and Chemical Biology at Northeastern University in Boston, Massachusetts.
Roxana E. Iacob is a Research Associate Professor at Northeastern University in Boston, Massachusetts. Her current research activities include the development and application of mass spectrometric techniques for biological applications, including improving the HDX-MS methodology and software to analyze large proteins and protein complexes in a more robust manner.
Ira S. Krull is a Professor Emeritus with the Department of Chemistry and Chemical Biology at Northeastern University in Boston, Massachusetts, and a member of LCGC’s editorial advisory board.
Anurag S. Rathore is a professor in the Department of Chemical Engineering at the Indian Institute of Technology in Delhi, India.
Articles in this issue
over 8 years ago
Method Adjustment the USP Wayover 8 years ago
UHPLC, Part I: Perspectives and Instrumental Featuresover 8 years ago
Vol 35 No 6 LCGC North America June 2017 Regular Issue PDFNewsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.