- The Column-04-16-2018
- Volume 14
- Issue 4
Investigating the Role of Amino Acids in Celiac Disease Development
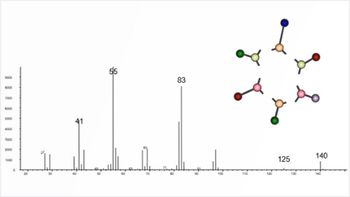
Researchers from the University of Gothenburg, in Gothenburg, Sweden, have investigated whether plasma amino acid levels differed among children with celiac disease using liquid chromatography–mass spectrometry (LC–MS) (1).
Researchers from the University of Gothenburg, in Gothenburg, Sweden, have investigated whether plasma amino acid levels differed among children with celiac disease using liquid chromatography–mass spectrometry (LC–MS) (1).
In the most recent decades the profile of celiac disease has risen immensely with the number of sufferers increasing thanks to improved diagnostics and recognition. The plight of sufferers has also became better known, and more recently their specialized diet has been subverted as a fad weight loss diet-further increasing the disease’s profile. Characterized by an intolerance to gluten, those suffering from celiac disease experience severe gastrointestinal distress in the form of abdominal pain and distension, diarrhoea, flatulence, nausea, and fatigue. However, celiac disease is not a mere food allergy. Both the innate and adaptive immune pathways are triggered, resulting in antibodies that target both gluten and the body’s own proteins causing damage to the intestinal mucosa. As such, the disease is generally considered an autoimmune condition.
Excluding gluten from the diet allows the damaged intestines of sufferers to repair, however, the mechanisms by which autoimmunity can be switched on and off by gluten intake still remain unresolved. Furthermore, what causes people to develop the disease in the first place remains unknown. Genetics appear to play a role because almost all diagnosed patients have mutations in two specific genes that allow the immune system to distinguish self from non-self and coordinate T-cell activity. However, these genetic factors appear to only partially dictate the pathogenesis because around 40% of people have these genes and yet not all go on to develop celiac disease (2).
In a previous paper, researchers carried out a Genome Wide Association Study (GWAS), which identified links towards genes involved in nutrient and amino acid signalling (3). Amino acid profiles have a well-established role in other chronic diseases such as type 2 diabetes (4–7), Alzheimer’s disease (8), or autism (9), where sufferers often have different amino acid profiles to those who are healthy. Several of the genes identified in the GWAS belonged to the Target of Rapamycin (TOR) pathway (10), a well-studied signalling pathway connecting amino acid signalling and immunity. Furthermore, the study revealed a connection between extra cellular matrices, which can act as a storage reservoir for certain amino acids, and celiac disease. The researchers hypothesized that certain amino acids, released following the breakdown of gluten, were involved in the signalling pathway of the immune system and ultimately led to chronic inflammation.
To investigate, researchers analyzed blood samples from children with and without the disease using LC–MS. The study found that children with untreated celiac disease had increased levels of seven amino acids when compared to healthy children. These findings suggest that the metabolism of amino acids could be responsible for the inflammation experienced by those with celiac disease. However, it is still unclear if these increased levels of amino acids are a result of the inflammation and not the cause. It could also be the case that the increased levels of amino acids are the result of a genetic predisposition in combination with environmental risk factors. Future studies are required to investigate these possibilities and fully understand where increased levels of amino acids fit within celiac disease pathogenesis. - L.B.
References
- Å.T. Naluai et al., PLoS ONE13(3), e0193764 (2018).
- https://www.the-scientist.com/?articles.view/articleNo/49467/title/The-Celiac-Surge [Accessed 24/03/18]
- M. Östensson et al., PLoS One8, (2013).
- Y. Zhou et al., Clin. Biochem.46, 1447–1452 (2013).
- H. Nakamura et al., Nurt. Diabetes 4, e133 (2014).
- B.A. Menge et al., Regul. Pept. 160, 75–80 (2010).
- E.P. Wijekoon, C. Skinner, M.E. Brosnan, and J.T. Brosnan, Can. J. Physiol. Pharmacol.82, 506–514 (2004).
- A.N. Fonteh et al., Amino Acids32, 213–224 (2007).
- S. Aldred et al., J. Autism Dev. Disord.33, 93–97 (2003).
- S.G. Dann and G. Thomas, FEBS Letters 2821–2829 (2006).
Articles in this issue
almost 8 years ago
Trends and Developmentsalmost 8 years ago
Agilent and Imperial College London Announce Collaborationalmost 8 years ago
Comprehensive Proteomic Analysis of Dog Salivaalmost 8 years ago
Solving the Problem or Merely Addressing the Issue?almost 8 years ago
Automated Determination Solution Viscosity of Polymeric Materialsalmost 8 years ago
Vol 14 No 4 The Column April 2018 Europe and Asia PDFalmost 8 years ago
Vol 14 No 4 The Column April 2018 North American PDFNewsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.