- LCGC North America-08-01-2010
- Volume 28
- Issue 8
Biosimilars: Introduction, Concerns, and Opportunities

The authors provide an introduction to the topic of biosimilars, review the available regulatory guidance, and discuss the various scientific challenges that are present.
The ever-increasing cost of healthcare and improvements in our understanding of the various factors that play a role in the manufacturing of biotech therapeutic drugs have fueled the push for approval of biosimilars (referred to as follow-on protein products in the U.S.). Discussion and resolution of the various scientific and regulatory factors behind the approval of biosimilars is perhaps one of the most significant events in the last decade for biotechnology. Reasons for this are many. For one, biotech processes and products are complex, and while the industry has made significant improvements in our understanding of how the process impacts the product, a lot more must occur. The use of complex feed materials that sometimes have not been fully characterized can further exacerbate this balance. Further, our understanding of how the product quality attributes impact the safety and efficacy of the product in the clinic is incomplete. This can be attributed to the complexities of the human body and is confirmed by the countless examples in the literature of observing significant changes in clinical performance (often undesirable) resulting from otherwise minor changes to the manufacturing procedures. In view of the difficult job that the regulatory agencies have in balancing the financial benefits with public safety, the European Medicinal Agency (EMEA) has done a commendable job at creating the regulatory path to facilitate approval of biosimilars. The U.S. Food and Drug Administration (FDA) is expected to do the same in near future.
In this column, we wish to provide our readers with an introduction to the topic of biosimilars, review the available regulatory guidance, discuss the various scientific challenges that are present, and talk about the opportunity that this provides to the drug manufacturers, regulators and the patients.
What are Biosimilars?
Biosimilars can be defined as biotech drugs that have been shown to have comparable quality, safety, and efficacy to the original product. There are some key differences between the production of biosimilars and that of the traditional small molecule generics:
Different Economics: Cost of manufacturing a biotech product is approximately 5–10 times more than that for a small molecule product. Capital investments as well as operating costs associated with manufacturing of biosimilars are also significantly higher than that for small molecule generics along with the associated risk of failure.
- Data on the launch of biosimilar epoteins in Germany shows that biosimilars represent approximately 35% of the total sales of epoetin (4). This is in comparison to much higher substitution rates than are seen for generic small molecule drugs (can exceed 90%).
- Biosimilars are expected to be priced at a 20–25% discount in comparison to the original products. This discount is significantly smaller than what is seen in the small molecule generics and reflects the intricacies associated with production and characterization of biotech products.
Complex processes: The impact of changes to manufacturing processes can cause significant change in efficacy or immunogenicity of the drug in the clinic.
Complex products: Biosimilars are larger, more complex molecules with associated structural heterogeneities (21). These heterogeneities are a result of activities in the host cell that are used to express the product, the bioreactor conditions under which the cells are grown, and the purification process utilized for generating the final product. Biotech products cannot be completely characterized analytically; that is, the analytical tools alone cannot predict behavior in the clinic.
Complex raw and feed materials: Feed materials used in manufacturing of biotech products tend to be complex, sometimes are not characterized, and sometimes are known to impact process consistency and product quality significantly.
Lack of understanding of relationship between product and process: The correlations between the clinical safety and efficacy of a biotech product and its product quality attributes generally are not known completely. So far, the clinical data have been mandatory so as to enable evaluation of safety and efficacy of the biosimilar drug in comparison to the original drug.
Opportunities
Healthcare is already one of the largest expenses for developed societies (U.S., Europe, and Japan) and is slowly becoming a concern for emerging economies as well. While the cost of biotech therapies is at present a relatively small portion of the total healthcare expense in the U.S. (which is by far the largest market for biotech drugs), this is expected to grow to about 30% (a 20-fold increase) in the next 10 years (8). This is likely to continue the pressure on the FDA to devise the regulatory pathway that would allow for review and approval of biosimilars. One study has suggested that as much as $2 billion can be saved by the European healthcare providers by just the first wave of biosimilar products (17). The regulatory authorities in Europe have already approved biosimilars for recombinant somatropin, recombinant human epoetin alfa, and recombinant filgrastim.
In a recent article, the authors concluded that as the analytical methodology becomes increasingly sophisticated, it is likely that manufacturers will consider biosimilar monoclonal antibody products (30). However, the authors also cautioned that the comparative trials that might be necessary to establish efficacy and safety of the biosimilar product versus the innovator product could be prohibitively large, making the idea of producing biosimilar monoclonal antibody products not feasible. The launch of Reditux (biosimilar of Genentech's Rituxan) by Dr. Reddy's laboratory in India seems to suggest that the possibilities do exist (6).
Regulatory Guidance and Issues
The European regulatory authorities already have established the framework for approval of follow-on protein products and have issued several key guidelines in this regards. The "Guideline on Similar Biological Medicinal Products" states that comparability studies are needed to establish similarity with respect to quality, safety, and efficacy of the biosimilar molecule with the innovator product (9). The "Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Quality Issues" lays down the quality requirements for a biosimilar product and addresses requirements regarding manufacturing process, comparability exercise, and choice of reference product, analytical methods, physicochemical characterization, biological activity, purity, and specifications of the biosimilar product (10). "The Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non-Clinical and Clinical Issues" lays down the relevant requirements for a biosimilar product and addresses requirements regarding pharmacokinetic, pharmacodynamic, efficacy studies, as well as the risk management plan (11). Finally, the "Annexes to Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non-Clinical and Clinical Issues – Guidance on Similar Medicinal Products Containing Somatropin, Recombinant Erythropoietins, Recombinant Granulocyte-Colony Stimulating Factor, Recombinant Human Soluble Insulin" provides guidance on nonclinical and clinical requirements for the specific products (1–4). "The Guideline on Immunogenicity Assessment of Biotechnology-Derived Therapeutic Proteins" states that immunogenicity evaluation should include data systematically collected from sufficient number of patients with the sampling schedule determined on a case-by-case basis, taking into account the risks associated with unwanted immune response to patient (12). "The Note for Guidance on Planning Pharmacovigilance Activities" recommends that a Safety Specification and Pharmacovigilance Plan be submitted at the time of license application that outlines the design and conduct of observational studies (16).
The FDA's scientific reasoning and experience in the area of follow-on protein products has been published recently via examples of FDA's actions involving the evaluation of various types of follow-on and second generation protein products and within-product manufacturing changes (29). A regulatory path for approval of follow-on protein products in the U.S. has yet to be proposed with the FDA Policy on Coordinated Framework for Regulation of Biotechnology governing the review and approval process of new protein products at present (FDA Policy).
Other organizations such as the World Health Organization (WHO) are also in the process of issuing guidelines that provide globally acceptable principles for licensing biotherapeutic products that are claimed to be similar to biotherapeutic products of assured quality, safety, and efficacy that have been licensed based on a full licensing dossier (28).
Challenges
The two major concerns with respect to approval and use of biosimilars are the efficacy and safety of the biosimilars in comparison to the original drug. In this section, we briefly present some of the key aspects that impact process and product comparability (7).
Relationship between the process and the product: Biotech products are known to be very sensitive to changes in manufacturing process. It is often said that "the process defines the product." An example of how changes in manufacturing process can impact the drug's clinical performance is the case of commercialization of interferon-b-1a for multiple sclerosis (24). The clinical material for Phase III study and the commercial material that had prior marketing approval from EMEA were made using the same gene, formulation, and storage conditions. They were delivered with the same dose, route, and frequency; and they were shown to have in vitro and in vivo comparability. However, because the two materials were made at two different sites with two different manufacturing processes, the Phase III material resulted in five times higher incidences of neutralizing antibodies than the material on the market.
Figure 1: Comparison of activity index for 11 non-innovator epoetin products available outside of US and Europe. Bioactivity was determined via an in vivo bioassay in mice. Activity index was calculated as the ratio of actual bioactivity divided by the bioactivity listed on the product. (Adapted from reference 25.)
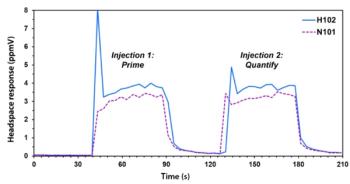
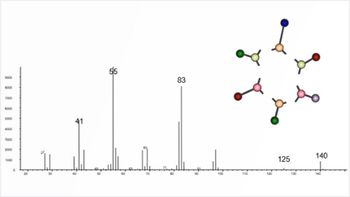
In view of this, the biosimilar manufacturer has to demonstrate its capability to control the process so as to manufacture product of consistent quality (5). This is followed up by a thorough comparison between the biosimilar and the innovator's product based upon thorough analytical examination (via a collection of high-resolution, orthogonal techniques), stability studies, nonclinical studies (such as receptor-binding studies and cell-based assays), and clinical studies (for pharmacokinetic, pharmacodynamic, and immunogenic behavior) (22). In all likelihood, the biosimilar product will differ from the innovator's product in a subsection of the quality attributes. As the effect of these differences on the clinical performance is not known completely, clinical safety needs to be monitored not only before giving approval but also postapproval. This is best illustrated by a comparison provided in Figure 1 that shows the activity index of 11 epoetins compared to Eprex (25). The activity index was calculated as the ratio of the bioactivity as determined by in vivo bioassay in mice and that in the specifications of the drug. A couple of observations can be made from this data. First, the activity index varies widely (0.71–2.26). Second, if we compare the variability to the conventional benchmarks (0.8–1.2), we find that two of the products (in red) seem to have less bioactivity than the lower end of the benchmark and four of the products (in dark blue) have more bioactivity than the upper end of the benchmark. It is evident from this data that for biosimilars to be approved successfully, the manufacturers will need to improve product quality. A similar comparison, also on epoetins, has been made (19) and is shown in Figure 2. The observations are similar to that in Figure 1 as some of the samples tend to fail the specifications for product concentration (80–120%, Figure 2a), pH (6.6–7.2, Figure 2b), and osmolarity (200–300 mOsm/kg, Figure 2c).
Figure 2: Comparison of (a) measured concentration, (b) pH, and (c) osmolarity of different rHuEPO samples from Asian market. (Adapted from reference 19.)
It can be inferred from the previous examples that to have consistent product quality, biosimilar manufacturers need to understand their processes and the interrelationships between the process parameters and product quality attributes (13,31). These principles also have been outlined in the emerging initiative of Quality by Design (15,20,21). However, biotech processes are complex and gaining this process understanding is a challenge due to the large number of process parameters and the quality attributes that can be interrelated (22). Figure 3a illustrates that as the number of factors being examined increases, the number of experiments required (to fully understand the impact of each factor and the interactions between them) increases much more rapidly, and this very soon becomes too large to conduct in a time- and resource-efficient manner. Further, Figure 3b illustrates the case of a typical process chromatography step that is used commonly in purification of protein products. Such a step can use >10 different raw materials and have >10 input parameters that can be altered during performance of the step. With >20 possible variables that can impact the performance for such a step, it is evident from Figures 3a and 3b that it is not possible to understand completely the impact of each raw material or input parameter on the performance of the unit operation. Use of risk assessment tools such as "Failure Mode and Effects Analysis" is used commonly to prioritize these variables into a reasonable number that can be examined via small-scale studies (13,26,31). High-throughput process development tools also are useful in achieving this objective in a time- and resource-efficient manner.
Figure 3: (a) Illustration showing the exponential increase in the number of experiments required with the number of factors that are being investigated in a full-factorial design of experiments (DOE) study. (b) Number of steps, raw materials, input parameters, and output parameters for a typical process chromatography step. The figure illustrates the complexity of unit operations utilized in manufacturing of protein products.
Relationship between the product and the clinic: Biotech products tend to be complex and subject to a lot of potential modifications, as listed in Table I (22,27). These include: desired process modifications such as pegylation; desired host cell modifications such as glycosylation, phosphorylation, sulfation, and acylation; undesirable host cell-related modifications such as truncation, acylation, glycation, and methylation; and undesirable process modifications such as aggregation, oxidation, and deamidation. Each of these modifications potentially can impact safety and efficacy of the product. In addition to the product-related modifications, there are numerous host cell-related impurities (host cell proteins, DNA, viruses, and so forth) and process-related impurities (antifoam, extractables, leachables, and so forth) that can be present in the final product. Glycosylation of proteins has been known to impact the drug's efficacy and stability, as well as the immunogenicity. Changes in degradation of the drug can produce novel antigenic epitopes, which in turn can result in changes to immunogenicity and metabolic half-life. The glycosylation pattern is a function of the host cell (microbial, insect, mammalian, and so forth) and the operating conditions of the bioreactor. Understanding how aggregate species interact with the immune system to enhance immune responses has been the focus of a recent review (23). The author suggests that the highly arrayed protein antigens, such as those present in nondenatured aggregate species, are capable of inducing antibody responses even in the absence of any help from the T-cells. Use of animal models and studies in understanding the effects of protein aggregates also was discussed. Host cell impurities, such as host cell proteins, DNA, and endotoxin can impact immunogenicity of the drug significantly. Endotoxins have been known to signal T-cells, resulting in activation of the B-cells and an immune response to the drug.
Table I: Illustration of the various quality attributes (QA) that need consideration during production of a biotech product and the various analytical tools that are used for characterization of the QA. The list is not intended to be exhaustive and is rather being presented to highlight the diversity of attributes and analytical methods. Adapted from 22.
Also shown in Table I is the gamut of high-resolution, orthogonal analytical tools that often are utilized to characterize some of these species. For example, protein aggregates often are considered a critical quality attribute due to their potential impact on immunogenicity of the drug, and these are characterized by multiple analytical techniques including capillary electrophoresis (CE), high performance liquid chromatography (HPLC), analytical ultracentrifugation (AUC), and light scattering. This enables a thorough comparison of the biochemical characteristics of the follow-on protein product versus the reference product.
Our lack of understanding of how the product quality attributes impact a biotech drug's safety and efficacy in the clinic is best illustrated by the case of Eprex. Use of this product for treatment of anaemia in patients with renal dysfunction has been associated with a higher incidence of pure red cell aplasia (PRCA), which is a severe form of anemia accompanied by near stoppage of production of the red blood cells. While it is not clear what triggered PRCA in this case, the two most common hypotheses include the change in formulation (from human serum albumin to polysorbate 80) and the presence of leachates from the uncoated rubber syringe stoppers into the drug (7). This example illustrates our limited understanding of biotech products with respect to which attributes drive their safety and efficacy.
Path Forward
With all the challenges that come with manufacturing and commercialization of biosimilars, the very significant cost savings that are likely to emerge from their approval is likely to serve as the motivation for the regulatory authorities to create a path that allows for examination and approval of biosimilars (in the U.S.) or continue on the path that has been laid out already (in Europe). The regulators have the daunting task of keeping the balance between the financial benefit from allowing approval of biosimilars and the safety of the patients. It is expected that while the topic of approval of biosimilars will stay controversial, decisions will need to be taken on a case-by-case basis and would depend upon a multitude of factors, as illustrated in Figure 4. The more we understand the starting materials and how they impact the performance of the process, the critical process parameters (CPP) of the process that impact the quality attributes of the product, and the critical quality attributes of the product that impact safety and efficacy in the clinic, the less we will rely on the clinical studies (assuming that comparability with respect to the relevant attributes has been demonstrated). It should be evident from the discussion here that generic approaches that have been taken for small molecules are not sufficient for protein products, even more so for complex biotech products, such as monoclonal antibodies.
Figure 4: Illustration of some of the significant factors that come into play when comparing a follow-on protein product to the parent molecule. The two extremes are shown in color. Green represents the case of minor process changes (improvements) that may be undertaken by the sponsor of an already licensed product. If the scope of the changes is sufficiently small, no clinical studies may be required. Red represents the case of filing a new biologic product with no predecessor, and thus, requires a full clinical dataset to support the drug’s safety and efficacy. Follow-on protein product applications will be in the middle of these two extremes with the answers to the presented questions driving the expectations from the regulatory agencies.
A recent paper has proposed some solutions for the aforementioned challenges (22). Postapproval pharmacovigilance will continue to play a critical role, as the clinical database is likely to be limited for biosimilars at the time of approval. In the preapproval period, only a few patients might receive the product in a relatively limited time period compared to the number of patients that will use the product during its complete lifecycle. The postapproval pharmacovigilance program needs to address the potential risks that often are associated with biotech drugs, especially immunogenicity. EMEA provides specific guidance on this subject (16), and often, these plans are part of the postapproval commitments that the biosimilar manufacturer makes to the regulatory agency.
Ira S. Krull Ira S. Krull "Validation Viewpoint" Co-Editor Ira S. Krull is an Associate Professor of chemistry at Northeastern University, Boston, Massachusetts, and a member of LCGC's editorial advisory board.
Anurag S. Rathore Anurag S. Rathore is a biotech CMC consultant and an associate professor with the Department of Chemical Engineering, Indian Institute of Delhi, India. He is also a member of BioPharm International's editorial advisory board.
References
(1) Annex Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non Clinical and Clinical Issues – Guidance on Similar Medicinal Products Containing Somatropin. Committee for Medical Products for Human Use. EMEA/CHMP/94528/05 (CHMP adopted February 2006).
(2) Annex Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non Clinical and Clinical Issues – Guidance on Similar Medicinal Products Containing Recombinant Erythropoietins. Committee for Medical Products for Human Use. EMEA/CHMP/BMWP/94526/2005 (CHMP adopted March 2006).
(3) Annex Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non Clinical and Clinical Issues – Guidance on Similar Medicinal Products Containing Recombinant Granulocyte-Colony Stimulating Factor. Committee for Medical Products for Human Use. EMEA/CHMP/BMWP/31329/2005 (CHMP adopted February 2006).
(4) Annex Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non Clinical and Clinical Issues – Guidance on Similar Medicinal Products Containing Recombinant Human Soluble Insulin. Committee for Medical Products for Human Use. EMEA/CHMP/BMWP/32775/2005 (CHMP adopted February 2006).
(5) A.J. Chirino and A. Mire-Sluis, Nat. Biotech. 22, 1383–1391 (2006).
(6) Company website.
(7) A. Covic, Nephrol. Dial. Transplant. 23, 3731–3737 (2008).
(8) M.R. Gillick, J. Am. Geriatr. Soc. 54, 1442–1446 (2006).
(9) Guideline on Similar Biological Medicinal Products. Committee for Medical Products for Human Use. CHMP/437/04 (CHMP adopted September, 2005).
(10) Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Quality Issues. Committee for Medical Products for Human Use. EMEA/CHMP/BWP/49348/05 (CHMP adopted February, 2006).
(11) Guideline on Similar Biological Medicinal Products Containing Biotechnology-Derived Proteins as Active Substance: Non-Clinical and Clinical Issues. Committee for Medical Products for Human Use. EMEA/CHMP/42832/05 (CHMP adopted February, 2006).
(12) Guideline on Immunogenicity Assessment of Biotechnology-Derived Therapeutic Proteins. Committee for Medical Products for Human Use. EMEA/CHMP/BMWP/14327/2006 (CHMP adopted December, 2007).
(13) J. Harms et al., Biotechnol. Prog. 24, 655–662 (2008).
(14) J. Hofgson, Nature Biotechnol. 27, 963–965 (2009).
(15) S. Kozlowski and P. Swann, "Considerations for biotechnology product Quality by Design," in Quality by Design for Biopharmaceuticals, A.S. Rathore and R. Mhatre, Eds. (Wiley Interscience, New York, 2009), pp. 9–30.
(16) Note for Guidance on Planning Pharmacovigilance Activities. CPMP/ICH/5716/03 (CHMP adopted December, 2004).
(17) P. O'Donnell, Appl. Clin. Trials 15, 38–42 (2006).
(18) Office of Science and Technology Policy, Coordinated Framework for Regulation of Biotechnology, United States Regulatory Agencies Unified Biotechnology website [online],
(19) S.S. Park, J. Pharm. Sci. 98, 1688–1699, (2009).
(20) A.S. Rathore and H. Winkle, Nature Biotechnol. 27, 26–34 (2009).
(21) A.S. Rathore, Trends Biotechnol. 27, 546–553 (2009).
(22) A.S. Rathore, Trends Biotechnol. 27, 698–705 (2009).
(23) A. Rosenberg, AAPS J. 8, E501–E507 (2006).
(24) R.A. Rudick et al., Neurology 50, 1266–1272, (1998).
(25) H. Schellekens, Eur. J. Hosp. Pharm. Sci., 3, 4347 (2001).
(26) R.J. Seely and J. Haury, Applications of failure modes and effects analysis to biotechnology manufacturing processes, in Process Validation in Manufacturing of Biopharmaceuticals, A.S. Rathore and G. Sofer, Eds. (Taylor & Francis, Boca Raton, Florida, 2005), pp. 13–30.
(27) P.G. Swann et al., Current Opinion Immunol. 20, 493–499 (2008).
(28) WHO Guideline on evaluation of similar biotherapeutic products (SBPs). 2009.
(29) J. Woodcock et al., Nat. Rev. Drug Discovery 6, 437–442 (2007).
(30) C.K. Schneider and U. Kalinke, Nature Biotechnol. 26, 985–990 (2008).
(31) P. van Hoek, J. Harms, X. Wang, and A.S. Rathore, Case Study on Definition of Design Space for a Microbial Fermentation Step, in Quality by Design for Biopharmaceuticals: Perspectives and Case Studies, A.S. Rathore and R. Mhatre, Eds. (Wiley Interscience, Hoboken, New Jersey, 2009) 85–109.
Articles in this issue
over 15 years ago
System Contaminationover 15 years ago
Why Does It Take So Long To Validate a Chromatography Data System?over 15 years ago
The Use of Hollow Fibers in Liquid-Phase Microextractionover 15 years ago
The "Chrommunity" Welcomes Two Distinguished New Membersover 15 years ago
Vol 28 No 8 LCGC North America August 2010 Regular Issue PDFNewsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.